|
Chronic compartment syndrome of the quadriceps femoris muscle in athletes. Diagnosis, imaging and treatment with fasciotomy. MATERIAL AND METHODS. RESULTS AND CONCLUSIONS. |
Alle indlæg af urtehave_com
treatment-article
|
Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. DESIGN. SETTING. PARTICIPANTS. INTERVENTIONS. MAIN OUTCOME MEASURES. RESULTS. CONCLUSIONS. |
examination-article
|
Intracompartmental pressure before and after fasciotomy in runners with chronic deep posterior compartment syndrome. |
step4
Training ladder for:
MUSCLE RUPTURE IN THE POSTERIOR THIGH
(RUPTURA MUSCULI)
STEP 4 |
Unlimited: Cycling. Swimming. Running and spurting.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
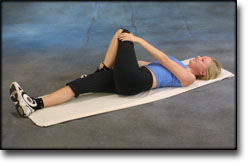
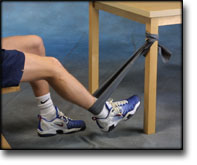
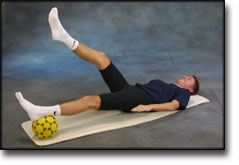
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step3
Training ladder for:
MUSCLE RUPTURE IN THE POSTERIOR THIGH
(RUPTURA MUSCULI)
STEP 3 |
Unlimited: Cycling. Swimming. Running with increasing speed.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
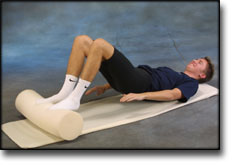
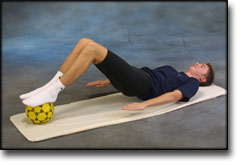
step2
Training ladder for:
MUSCLE RUPTURE IN THE POSTERIOR THIGH
(RUPTURA MUSCULI)
STEP 2 |
Unlimited: Cycling. Swimming. Jogging.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
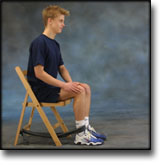
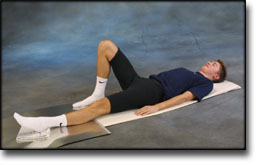
step1
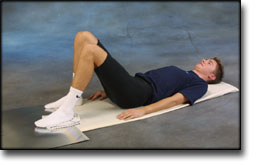
Training ladder for:
MUSCLE RUPTURE IN THE POSTERIOR THIGH
(RUPTURA MUSCULI)
STEP 1 |
| The indications of time after stretching, coordination training and strength training show the division of time for the respective type of training when training for a period of one hour. The time indications are therefore not a definition of the daily training needs, as the daily training is determined on an individual basis.
|
|||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
treatment-article3
|
Anterior compartment syndrome of the thigh in athletes–indications for conservative treatment. |
treatment-article2
|
Acute compartment syndrome. |
treatment-article1
|
Thigh compartment syndrome in a football athlete: a case report and review of the literature. |