|
Incidence and causes of tenosynovitis of the wrist extensors in long distance paddle canoeists. METHOD. RESULTS. CONCLUSION. |
Alle indlæg af urtehave_com
examination-article
|
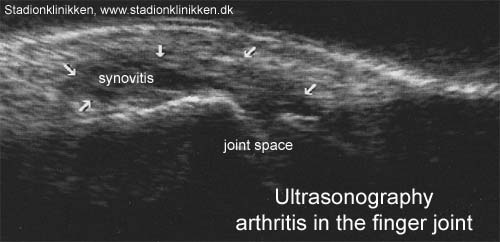
Usefulness of high resolution US in the evaluation of effusion in osteoarthritic first carpometacarpal joint. METHODS. RESULTS. CONCLUSIONS. |
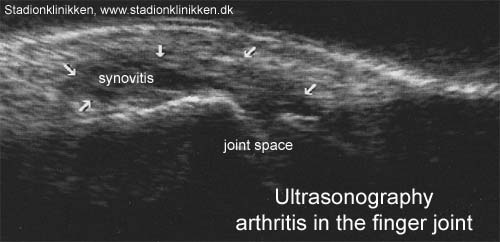
ultrasonic-image
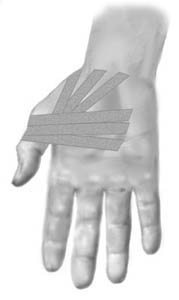
tape-instruction
Objective: Stabilise the metacarpophalangeal joint (MCP1 joint) |
|||
 |
|||
| Application: The thumb should be held in a neutral position. Start in the middle of the palm adjacent to the wrist, draw the tape around the thumb’s metacarpophalangeal joint and return to the palm and cross the start tape (A). The next tape is applied in similar fashion, but started slightly further out on the palm (B). A third strip can be applied in a continued fan formation. (C). |
treatment-article2
|
Role of MR imaging in the management of “skier’s thumb” injuries. |
treatment-article1
|
Sonography of the injured ulnar collateral ligament of the thumb. |
examination-article
|
The skier’s thumb. |

photo

step4
Training ladder for:
INFLAMMATION OF THE HOLLOW FOOT TENDON
(FASCIITIS PLANTARIS)
STEP 4 |
Unlimited: Cycling. Swimming.
|
||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step3
Training ladder for:
INFLAMMATION OF THE HOLLOW FOOT TENDON
(FASCIITIS PLANTARIS)
STEP 3 |
Unlimited: Cycling. Swimming.
|
||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |