|
Placement of intra-articular injections verified by ultrasonography and injected air as contrast medium.
Fredberg U, van Overeem Hansen G, Bolvig L. Ann Rheum Dis 2001 May;60(5):542.
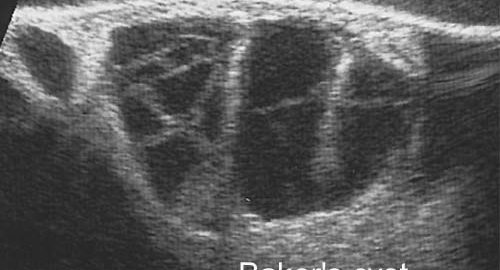
Intraarticular injection of long-acting corticosteroid is a corner stone in rheumatological treatment. The injected intra-articular corticoid is more effective when the placement is correctly secured. Injection of radiographic contrast material has shown that less than half of the injections are correct placed in the joint space after blind injection. Generally, the clinical application of ultrasonographic examinations can be enhanced by contrast agents. The most common used technique is creation of microbubble contrast agents. Such agents, applied to the bloodstream, have been used for hepatic, nephrologic, cardiologic and transcranial examinations. Obviously, the risk of air embolism depends on the anatomic site of the injected air contrast. Transient ischemic attacks are described after echocardiography with air contrast and in animal models haemodynamic effects during venous air infusion can be measured. Intra-articular injection of air and subsequently lateral and posterior radiographs has shown that this technique can enhance the procedure precision. The disadvantage of this method is that the result can first be seen after the injection, and that a correction can only be made with a new injection. In the joint space the air is separated from the vascular system and when only small amounts of sterile air are used the risk of venous air embolism is neglectable. Air is a very effective contrast medium in ultrasonography. Air sonography has been used for the diagnosis of meniscus lesions in knee joints and for rotator cuff lesions in the shoulder. We expand the applicability of this method to all joints, not only for diagnostic purposes, but also for the correct placement of the needle before injection of medicine (steroid, osmium-acid, viscosupplementation): The sterile air that is contained in the capped vial with lidocain or steroid is used as contrast medium. The needle is ultrasonographic guided placed in the joint space profound for the distended capsule. When the steroid and lidocain are mixed in the syringe a small volume of air will be in the needle itself (˜ 0.05 ml). The air in the needle is clearly seen when the injection is started and will secure the correct placement of the needle. With this technique, it is not necessary to use two separate syringes and the inclination of the syringe will not cause the air to move from the needle to the bottom of the syringe. If the knee is injected, injection directly into the recess is recommended, which will make the small volume of air possible to be seen momentary. Figure 1 illustrates the ultrasonography of a MTP joint in a patient before (UL-34A) and after (UL-34B) injected air. The intraarticular air is clearly seen. We had made more than one thousand ultrasonography guided intraarticular injection without any complications. This method is easy, inexpensive, without risk and radiation and should be used routinely in rheumatology. Especially chemical synovectomy of the knee should always be guided by ultrasonography and with this technique also smaller joins can be considered for chemical synovectomy.
|