| Instructions.
Rehabilitation begins with the exercises at Step-I. When the exercises at Step-I can be performed without pain (whilst performing the exercises, in the evening or next morning), the exercises at Step-II can be commenced. When the Step-II exercises can be completed without discomfort, the exercises at Step-III can be started, following on to Step-IV. If any soreness is experienced upon completion of the exercises which gives cause for any doubt as to whether this is due to normal muscle stiffness following training, or more of a “warning” soreness due to the intensity of the training increasing too quickly, the next training session should be performed on the same level. If the soreness subsequently diminishes, the soreness can be attributed to normal muscle stiffness, and the rehabilitation can be cautiously increased. If, on the other hand, the soreness does not decline, the rehabilitation is being forced too quickly, and the load has exceeded the limit which the injury is capable of managing for the time being. The training load and intensity should consequently be reduced immediately, and training should continue on a lower level for some days before being cautiously increased again. The amount of time which it is possible to use on the rehabilitation exercises naturally varies greatly from person to person, and the indications given should therefore be considered as a guideline for the relationship between strength, coordination and agility training, and can be amended according to the training opportunities which are available, as well as individual requirements. The rehabilitation period will generally pass quicker if more training is performed. However, if the guidelines in SportNetDoc go against information from your own doctor, you should naturally follow the advice of the doctor which has examined and evaluated your injury. The guidelines in Rehabilitation, general should be read before the exercises in Steps I-IV are commenced.
|
Alle indlæg af urtehave_com
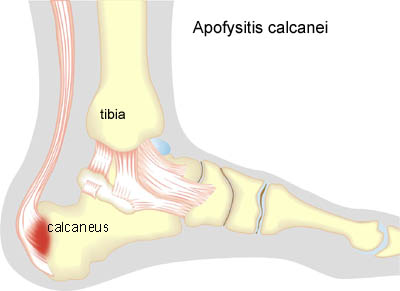
Inflammation of the growth plate of the heel bone (apophysitis calcanei)
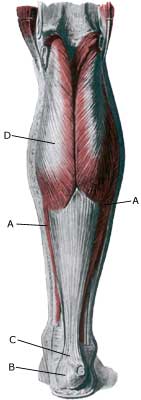
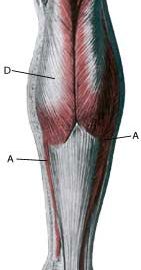
Anatomy: The calf muscle (M Gastrocnemicus) is comprised of two muscle heads which gather in a wide tendinous ligament and continue in to the Achilles tendon. Another of the larger calf muscles (M Soleus) is attached to the front side of the Achilles tendon and thus forms a part of the Achilles tendon. The Achilles is attached to the heel bone (calcaneus) where a growth zone is found in children represents the weakest area of the Achilles tendon and calf muscle in non-adult persons. |
||
|
||
 |
||
| Cause: Inflammation at the point of attachment of the Achilles tendon at the heel bone occurs with continued overload in the form of running and jumping.
Symptoms: Pain when activating the Achilles tendon (running and jumping) and with stretching of the tendon. Tenderness is experienced when applying pressure at the rear of the heel bone. Acute treatment: Click here. Examination: Medical examination is not necessarily required in slight, early cases where the tenderness is slowly increasing without sudden worsening. In all cases when there is a sense of a “crack”, or sudden shooting pains in the Achilles tendon, medical attention should be sought as soon as possible to exclude a (partial) rupture of the Achilles tendon. This situation is best determined by use of ultrasound scanning, as a number of injuries requiring treatment can easily be overlooked during a medical examination. A normal medical examination is usually sufficient in order to make the diagnosis, however, in all cases where satisfactory progress is not in evidence, an ultrasound examination should be performed as early as possible. Ultrasound scanning enables an evaluation of the extent of the change in the tendon; inflammation of the tendon (tendinitis), development of cicatricial tissue (tendinosis), calcification, inflammation of the tissue surrounding the tendon (peritendinitis), inflammation of the bursa (bursitis), as well as (partial) rupture and fraying of the bone membrane, as is often the case in children with inflammation at the point of attachment of the Achilles tendon at the growth zone on the heel bone (Photo) (article). Treatment: Treatment is primarily comprised of relief from the painful activity (running, jumping). If the treatment is commenced early, the injury can in some cases heal within a few weeks. When the pain has subsided, the sports activity can be resumed preceded by stretching and strength training of the calf muscle. Unfortunately the Achilles problems at the attachment (enthesopathy) are more difficult to treat by (eccentric) training than mid-portion Achilles tendinitis (article). It is naturally crucial that footwear is in good condition (good running shoes with shock absorbing heel and close fitting heel cap). Pressure on the Achilles tendon can be relieved by using shoes with an elevated heel, whilst a heel cushion in the shoe is of less significance since the heightening achieved by this method is greatly limited. If experiencing tenderness at the point of attachment of the Achilles tendon during the rehabilitation period, treatment with ice for a period of at least 20 minutes is recommended. To relieve pronounced pain whilst walking, medicinal treatment in the form of rheumatic medicine (NSAID) (gel or crème) can be considered in the acute stage but is seldom indicated in the chronic stage. Medicine must not be (mis)used in order to continue the sports activity. Injection of corticosteroid is not appropriate in the course of treatment in children (article) but can be used in adults. Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude: |
x-ray-artical
|
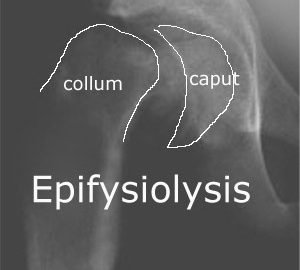
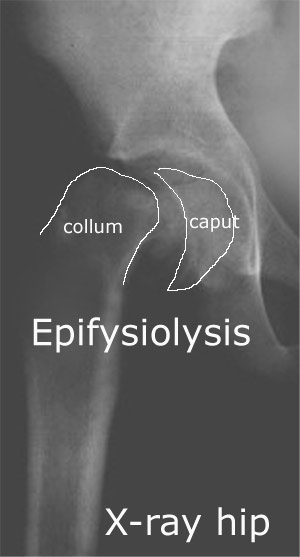
Diagnostic imaging of the early slipped capital femoral epiphysis. Magnano GM, Lucigrai G, De Filippi C, Castriota Scanderberg A, Pacciani E, Toma P. Radiol Med (Torino) 1998 Jan-Feb;95(1-2):16-20 |
x-ray
STEP4
Training ladder for:
SLIMSÆKSBETÆNDELSE VED ACHILLESSENEFÆSTET
(BURSITIS ACHILLES)
STEP 4 |
|
|||||||||||||||||||||||||||||||||||||||||||||
STEP3
Training ladder for:
SLIMSÆKSBETÆNDELSE VED ACHILLESSENEFÆSTET
(BURSITIS ACHILLES)
STEP 3 |
|
|||||||||||||||||||||||||||||||||||||||||||||
STEP2
Training ladder for:
SLIMSÆKSBETÆNDELSE VED ACHILLESSENEFÆSTET
(BURSITIS ACHILLES)
STEP 2 |
|
|||||||||||||||||||||||||||||||||||||||||||||
STEP1
Training ladder for:
SLIMSÆKSBETÆNDELSE VED ACHILLESSENEFÆSTET
(BURSITIS ACHILLES)
STEP 1 |
|
||||||||||||||||||||||||||||||||||||||||
Treatment-a2
|
Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. |
Treatment-a1
|
Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional achilles tendinosis with calcific spur. |