|
Treatment of proximal plantar fasciitis with ultrasound-guided steroid injection. DESIGN. SETTING. PATIENTS. INTERVENTION. MAIN OUTCOME MEASURES. RESULTS. CONCLUSION. |
Kategoriarkiv: Foot
treatment-article3
|
Treatment of proximal plantar fasciitis with ultrasound-guided steroid injection. DESIGN. SETTING. PATIENTS. INTERVENTION. MAIN OUTCOME MEASURES. RESULTS. CONCLUSION. |
Corticosteroids
| CORTICOSTEROIDS
Injection of corticosteroid in sports-medicine is used as a result of the following indications:
No other legal treatment of sports injuries has been so controversial as localised injection of corticosteroid. There is, however, no documentation that injection of corticosteroid in the area surrounding the tendons, in the joint or in the bursae should be harmful (article) (article). Although laboratory tests do indicate an immediately weakening in the tendon tissues shortly after the injection (article), human studies show no sign thereof (article). Injections direct into the tendons should be advised against however, as certain animal studies suggest that the tendon is thereby weakened (article). Indications. Arthritis (swelling of joints due to rheumatism). Injection of corticosteroid in the joint is one of the treatments most commonly used in rheumatic illnesses. Placebo controlled studies have documented the effect of this form of treatment. Mechanism of action. The mechanism of action is not fully clarified. Side effects. The risk of infection is minimal with the observance of simple sterile procedures (disinfection with surgical spirits at least twice, sterile equipment, “non-touch technique”). Bleaching of the skin above the infection with visible blood vessels in the skin, a change in the sensitivity of the area, and partial loss of fatty tissue are frequent occurrences, but only in very rare cases give any discomfort. The majority of discomfort disappears spontaneously after several months (years). The risk of systematic effect following injection of corticosteroid is shown by facial blushing (about 10 %), menstruational disorder and fluctuation of blood sugar which is seen quite frequently while serious side effects like allergic shocks are extremely rare. Erroneous injection direct into the tendons as well as injection surrounding partial (and total) ruptured tendons can occour. It is for this reason that ultrasound scanning is recommended prior to all injections in areas where there are large tendons (Achilles tendon, knee cap tendon, hollow foot tendon), to ensure the correct diagnosis and exclude partial ruptures. If injections are given under the guidance of ultrasound, it will ensure the correct injection and optimal effect whilst minimising the risk. The athlete should be advised of the risk of tenderness in the area for a while after the injection (fading away during the course of a few hours or days). Local treatment with corticosteroids is allowed by the doping law. Contraindications. Suspicions of infection in the vicinity of the place of injection and active tuberculosis. As there is only modest experience of the effects of corticosteroid injections on children, this treatment is seldom indicated for minors. Administration. The corticosteroid is mixed with local anaesthetic prior to injection, thereby reducing the risk of side effects. The temporary subduing of pain (due to the local anaesthetic) will furthermore aid the confirmation (or the disconfirmation) of the diagnosis. Systemic treatment (tablets, suppositories, injections in the muscles and veins for systemic effect) with corticosteroid is not permitted in sport. Discussion. Injections with corticosteroid in the area surrounding tendons can amongst other things be used as a supplement to treatment for chronic over-load conditioned tendon injuries. The basis treatment is “active rest” with increasing load within the pain threshold. If the athlete does not follow the rehabilitation principles and instead forces the rehabilitation, the chronic inflammation, the lengthy rest period and the suddenly increased training load will present a risk of rupturing the tendon. Conclusion. Localised injection of corticosteroid is considered effective as treatment for bursitis, chronic inflammation of the tendon (tendinitis), inflammation of the tendon sheath (tenosynovitis), inflammation of the tissue surrounding the tendons (peritendinitis) and fluid accumulation in the joints (traumatic arthritis/synovitis), although the scientific documentation is incomplete. Resumé. Medicinal treatment is only a supplement to the basis treatments of sport injuries. Used the right way, the medicinal treatment can reduce the relieving period thereby starting the rehabilitation faster. If the treatment is abused to continue a harming sports activity without corrective training measurements, the risk of chronic injuries will increase.
|
treatment-article(1&2)
|
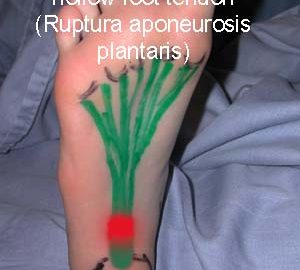
Plantar fascia rupture: diagnosis and treatment. |
Inflammation of the tendon (fasciitis plantaris)
|
||
|
||
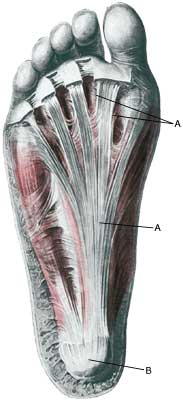
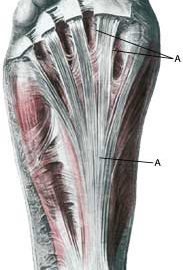
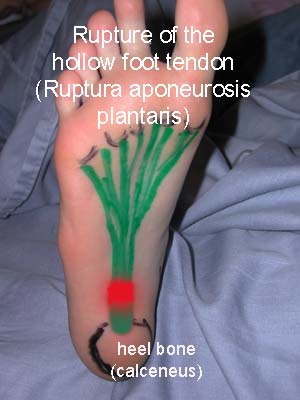
| Cause: Occurs after repeated overload in the form of running or jumping. Since the hollow foot tendon is a functional extension of the Achilles tendon, the provoking factors which are instrumental in injuries due to overload of the hollow foot tendon and the Achilles tendon are often the same.
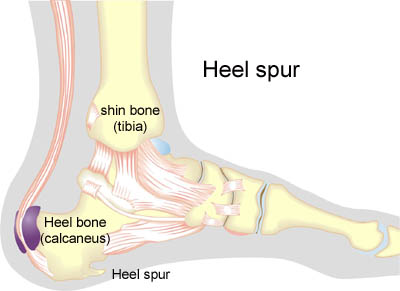
Symptoms: Pain when running and jumping, as well as when applying pressure at the attachment point of the hollow foot tendon directly under the heel bone. The pain is often most pronounced slightly on the inner side of the attachment. Acute treatment: Click here. Examination: Medical examination is not necessarily required in slight, early cases where the tenderness is slowly increasing without sudden worsening. A normal medical examination is usually sufficient in order to make the diagnosis, and in all cases when there is a sense of a “crack”, or sudden shooting pains in the tendon, medical attention should be sought as soon as possible to exclude a (partial) rupture of the hollow foot tendon and bone fracture. This situation is best determined by use of ultrasound scanning (or MRI examination), as a number of injuries requiring treatment can easily be overlooked during a clinical examination. In cases where satisfactory progress is not in evidence, an ultrasound examination should be performed as early as possible. Ultrasound scanning enables an evaluation of the extent of the change in the tendon; inflammation of the tendon (tendinitis), development of cicatricial tissue (tendinosis), calcification, inflammation of the tissue surrounding the tendon (peritendinitis), inflammation of the bursa (bursitis), as well as (partial) rupture (article) (Ultrasonic image). Treatment: Rest from the painful activity (running). The injury can in some cases heal within a few weeks if treatment is commenced at an early stage (article). If the pain has been present for several months, and especially if ultrasound scanning reveals thickening and change in the tendon, a rehabilitation period of several months must be anticipated. Special emphasis is laid upon strengthening exercise where the calf muscle is activated simultaneously with being stretched (eccentric training). It is imperative that the footwear is in order, with good running shoes including shock absorbing heels. Pressure on the hollow foot tendon can be relieved by walking in shoes with an arch support. Treatment with ice can be repeated every time the hollow foot tendon becomes tender during the rehabilitation phase. If satisfactory progress is not made in the training, medical treatment can be considered in the form of rheumatic medicine (NSAID) or injection of corticosteroid in the area around the thickened part of the tendon. Ultrasound guided injection increases the effect of the injection, as well as reduces the risks involved. Research has shown that ultrasound guided injections of corticosteroid are extremely effective in reducing the extent of the thickened tendons, to enable more active rehabilitation to commence (article). As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or rupture. It is not unusual for a rehabilitation period of six months before maximum strain or load in the form of jumping is permitted. The tendon is naturally unable to accommodate maximum strain or load after a prolonged injury period after only a short rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected (article). During recent years, different types of experimental treatment have been seen such as shock-wave (ultrasound treatment). However, there is no sure or clear documentation for the effect of the treatment. If the rehabilitation and conservative treatment does not yield progress, surgical intervention can be attempted. The long term results of operations are often disappointing (article-1), (article-2), (article-3). Heel spur: Inflammation of the hollow foot tendon is occasionally connected to a heel spur. A heel spur is a new bone development which is seen in connection with a prolonged inflammation at the point of attachment of the hollow foot tendon on the heel bone due to overload. A heel spur is thus a consequence of an injury due to overload, and not the cause. If a heel spur has developed, it will never disappear. Heel spurs have no practical significance, and require no treatment. Many symptom free athletes have heel spurs without having had symptoms from the point of attachment of the hollow foot tendon. Surgical removal of heel spurs as performed in earlier days is now virtually no longer used
Bandage: Taping to relieve problems with the hollow foot tendon is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction). Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude:
Few sports injuries carry as large a risk of chronic, permanent sporting disability as inflammation of the hollow foot tendon. In the severe, chronic cases, all treatment and rehabilitation attempts will often result in permanent inability to continue the sports activity. Special: As prolonged overload or strain on the hollow foot tendon has a large risk of developing in to chronic inflammation, which is extremely difficult to treat, it is important to prevent the injury from arising or recurring. The principles in “Rehabilitation, general” should be followed to ensure that quickly increasing training loads at the season start, or after an injury period, are avoided. It is important that running shoes fit well (tight heel cap, shock absorbing soles ). It is vital that the first signs of tenderness or pain are reacted upon, to enable the training to be adapted before the injury reaches the stage where continuing the sports activity may be at risk. |
Anatomy(PHOTO)

Complications(x-ray 2)


Complications(x-ray 1)

Treatment
|
Treatment strategies for acute fractures and nonunions of the proximal fifth metatarsal. |

Cause(x-ray)