| Cause: Rupture of the hollow foot tendon occurs after sudden, forceful overload (for example landing after jumping). In a number of cases, a rupture of the hollow foot tendon is preceded by inflammation of the tendon (fasciitis plantaris). Since the hollow foot tendon is a functional extension of the Achilles tendon, the provoking factors which are instrumental in injuries due to overload of the hollow foot tendon and the Achilles tendon are often the same.
Symptoms: In light cases, a localised tenderness can be felt at the point of attachment of the hollow foot tendon under the heel bone, or under the arch of the foot after strain or load (“sprain”, “threatening muscle pull”). In more severe cases, sudden shooting pains can be felt in the tendon (“partial rupture”, “pulled muscle”) and at the worst a sensation of feeling and hearing a “crack” after which it is impossible to run and pain is felt whilst walking (“total tendon rupture”), where it is often possible to feel a defect in the hollow foot tendon. Total ruptures are very rare.
Acute treatment: Click here.
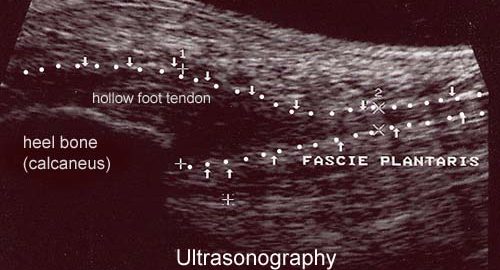
Examination: In all cases when there is a sense of a “crack”, or sudden shooting pains in the tendon, medical attention should be sought as soon as possible to make the diagnosis. Ultrasound scanning (or MRI examination) is used to advantage for making a swift and correct diagnosis, as injuries requiring treatment will often be overlooked under normal clinical examination (article).
Treatment: The chosen treatment will usually be relief until the pain disappears (article), and surgical intervention if the rehabilitation does not proceed satisfactorily (article). If a tender lump of cicatricial tissue develops after several months of rehabilitation (inflamed granuloma), treatment can be supplemented in medicinal form by rheumatic medicine (NSAID) or injection of corticosteroid in the area surrounding the inflamed lump of cicatricial tissue. Ultrasound guided injection increases the effect of the injection, as well as reduces the risks involved (article). As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or (further) rupture. The tendon is naturally unable to accommodate maximum strain or load after a prolonged injury period after only a short rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected (article-1) (article-2). It is not unusual for a rehabilitation period of six months before maximum strain or load in the form of jumping is permitted. It is vital for safety that injections are performed under guidance of ultrasound when treating chronic hollow foot tendon injuries.
Bandage: Taping to relieve problems with the hollow foot tendon is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction).
Prevention: As inflammation of the hollow foot tendon is extremely difficult to treat, it is important to prevent the injury from arising or recurring. The principles in rehabilitation, general should be followed to ensure that quickly increasing training loads at the season start, or after an injury period, are avoided. It is important that running shoes fit well (tight heel cap, shock absorbing soles). It is vital that the first signs of tenderness or pain are reacted upon, to enable the training to be adapted before the injury reaches the stage where continuing the sports activity may be at risk.
Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude:
In the severe, chronic cases, all treatment and rehabilitation attempts will often result in permanent inability to continue the sports activity.
Special: As there is a risk that the injury can cause permanent disability, all cases should be reported to your insurance company.
|