|
Intramuscular corticosteroid injection for hamstring injuries. A 13-year experience in the National Football League. Levine WN, Bergfeld JA, Tessendorf W, Moorman CT 3rd. Am J Sports Med 2000 May-Jun;28(3):297-300. The purpose of this study was to assess the safety of intramuscular corticosteroid injection in selected, severe hamstring injuries in professional football players. Clinicians have been reluctant to use corticosteroid injections in or around muscle-tendon units because of concern of incomplete healing or rupture. We retrospectively reviewed the computer database of one National Football League team for all hamstring injuries requiring treatment between January 1985 and January 1998. We found that 431 players had suffered such injury. We developed a clinical grading system to identify hamstring injury severity and to stratify players for treatment. Fifty-eight players (13%) sustained severe, discrete injuries with a palpable defect within the substance of the muscle and were treated with intramuscular injection of corticosteroid and anesthetic. There were no complications related to the injection of corticosteroid. Only nine players (16%) missed any games as a result of their injury. Final examination revealed no strength deficits, normal muscle bulk and tone, and the ability to generate normal power. We believe that the grading system we developed can assist in selection of injury type for injection. Although lack of a control group limits statements of efficacy of injection, our impression is that intramuscular corticosteroid injection hastens players’ return to full play and lessens the game and practice time they miss. |
Kategoriarkiv: General
MUSCLE RUPTURES ARTICLE2
|
Myositis ossificans of the upper extremity: a long-term follow-up. Carlson WO, Klassen RA. J Pediatr Orthop 1984 Nov;4(6):693-6. The long-term results of nonoperative treatment of myositis ossificans traumatica have been infrequently reported. We reviewed 83 cases of myositis ossificans seen at the Mayo Clinic from 1950 to 1979 in patients up to 21 years of age. The upper extremity was involved in 31 patients. Follow-up averaged 13 years for 23 of the (74%) patients studied. Football injuries had occurred in 20 of these patients, and the diagnosis was made an average of 3.3 weeks from the time of the initial injury. Observation was the only treatment in 18 of the 31 cases. At follow-up two-thirds of the patients with upper extremity involvement had no problems associated with the disorder, and one-third described some difficulties. Nonoperative treatment remains an accepted management approach for this problem. |
MUSCLE RUPTURES ARTICLE1
|
Treatment of traumatic myositis ossificans circumscripta; use of aspiration and steroids. Molloy JC, McGuirk RA. J Trauma 1976 Nov;16(11):851-7. The classification, clinical presentation, forms of treatment, and theories of pathogenesis of traumatic myositis ossificans circumscripta are reviewed. A group of 7 patients with this lesion was treated with hematoma aspiration and injection of steroids, lysosomal enzymes, and xylocaine, resulting in significant limitation of disability. The determining factor in the development of this disorder seems to be the response of local soft tissues to trauma rather than the magnitude of the trauma itself which we feel accounts for the success of the form of treatment described. |
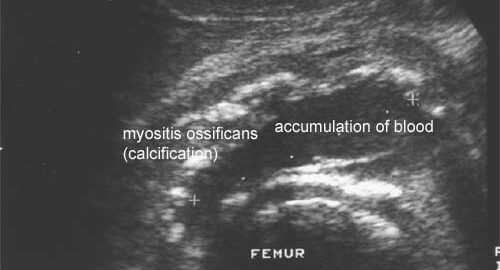
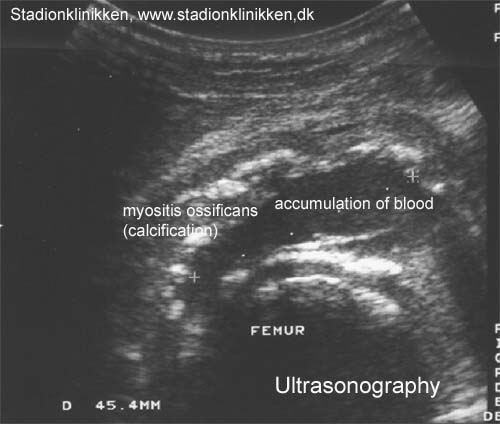
MUSCLE Ultrasonic image
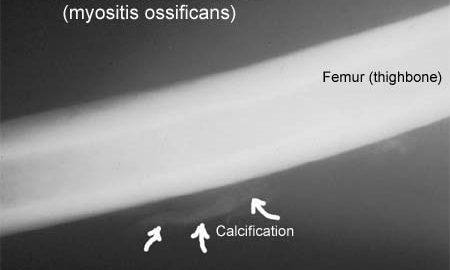
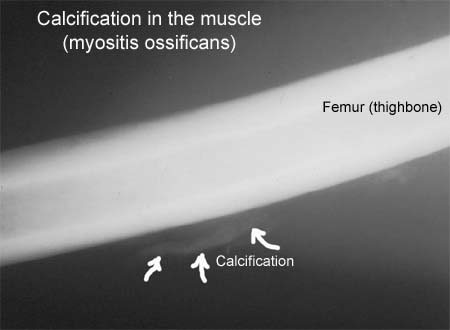
COMPLICATION OF MUSCLE X RAY PICTURE
COMPLICATION OF MUSCLE RUPTURES IN GENERAL
| COMPLICATION OF MUSCLE RUPTURES IN GENERAL: | |
| 1. | Calcification in the muscle (Myositis ossificans): Muscles which have been subjected to a rupture can from time to time be found to have some calcification, although the reasons for this are unknown. The diagnosis is often made due to the rehabilitation not progressing as expected in relation to the primary evaluation of the extent of the injury. The calcification can be seen under ultrasound scanning after a few days, and subsequently on an x-ray after a few weeks (X-ray picture), (Ultrasonic image) . The treatment comprises relief, and if possible, ultrasound-guided draining of the blood accumulation, ultrasound-guided injection of corticosteroid and rheumatic medicine (NSAID). A considerably longer rehabilitation period must be expected if the muscular bleeding is complicated by calcification in the muscle. Surgery is almost never indicated, as an operation can involve further calcification. Vigorous massage on the blood accumulation should be avoided on the same grounds (article-1), (article-2). |
| 2. | Formation of scar tissue in the muscles (cicatricial tissue). Formation of scar tissue is often seen after a muscle rupture, and can in some cases cause permanent discomfort. The formation of scar tissue is often the cause of the rehabilitation progressing slower than anticipated, as well as relapses a long time after the injury initially occurring. A local tenderness in the muscle can usually be experienced, aggravated when activating and stretching the muscle. It is often possible to detect scar tissue under ultrasound scanning, however, this can be quite difficult and requires a doctor well experienced in performing ultrasound scans. An area of inflammation will often be seen surrounding the scar tissue formation. The treatment comprises further relief, possibly supplemented by rheumatic medicine (NSAID) or ultrasound-guided injection of corticosteroid, (article). |
| 3. | Blood accumulation in the muscle (haematoma musculi). Injuries to muscles always involve muscular bleeding to a greater or lesser extent. In some cases the bleeding is diffuse between the muscle cells, whereas other cases can involve the bleeding being a larger, well-defined accumulation in the muscle. The larger the accumulation, the longer period is required for the accumulation to disappear and allow the muscle to heal. Accumulations of blood in the muscles often entail more pronounced pain than anticipated in relation to the primary evaluation of the extent of the injury. The diagnosis is best made via use of ultrasound scanning. If the accumulation is large it can be drained, which can advantageously be performed under guidance of ultrasound. Some recommend treatment with rheumatic medicine (NSAID) and advise caution regarding massage to reduce the risk of myositis ossificans. |
| 4. | Formation of fluid in the muscle (Hygrom). A formation of fluid will sometimes appear after an injury to a muscle, and can be of a considerable size. If the fluid does not diminish following relief, the accumulation can be drained by use of ultrasound scanning, with injection of corticosteroid being a further possibility. Fluid accumulations can be the cause of the rehabilitation not progressing smoothly. |
| 5. | Acute compartment syndrome: The groups of muscles on the arms and legs are surrounded by taught muscle membranes (fascias), which are partially unremitting. Damage to blood vessels and nerves can be caused if the bleeding and fluid accumulation in the muscles reaches such a size that the pressure in the muscle group increases. Serious damage to muscles can be caused in acute cases which result in the blood vessels closing. The symptoms comprise increasing pain in the damaged arm or leg muscle, which is often more powerful than expected from the primary evaluation of the extent of the injury. At the same time sensory disturbances can occur. The diagnosis is made by performing a pressure measurement in the muscle compartment, (article). The treatment comprises acute severing of the muscle membrane. It is imperative for the continuing function of the muscle that this operation will be acute, which is, of course, only possible if the athlete seeks acute medical attention, (article-1), (article-2), (article-3). |
| 6. | Chronic compartment syndrome: The groups of muscles on the arms and legs are surrounded by taught muscle membranes (fascias), which are partially unremitting. Pain can be experienced in a muscle group in the leg after only a few minutes activity following an earlier muscle injury, or following a very rapid increase in training of individual muscle groups. There is a sensation that the muscle is “tightened” and becomes hard, which is accompanied by discomfort. If the activity is stopped the discomfort diminishes, but returns a short period after the resumption of sports activity. This can be due to the muscle swelling up (after injury), or growing quicker than the muscle membrane can manage to keep up to (increase in training intensity too fast), whereby the pressure on the blood vessels and nerves in the muscle group increases. The diagnosis can be made with a pressure measurement in the muscle compartment, (article). Treatment comprises relief with slowly increasing training intensity after loss of symptoms, rheumatic medicine (NSAID). If there is scar tissue in the muscle, ultrasound guided injection of corticosteroid around the scar tissue formation can be attempted. In cases where there is a lack of progress a surgical severing of the muscle membranes can be performed, which is usually a minor procedure with good results. (article-1), (article-2). |
KNEE LATERAL STABILISATION
Objective: Stabilise the knee joint against too great a lateral twist (especially valgus twist) without reducing the normal mobility of the knee. The tape is utilised the whole day in the beginning of the course, being gradually reduced over the following three months. The tape is finally only used in connection with particular loads where there is risk attached. |
|||
 |
|||
| Application: The knee should be kept slightly bent (approx. 20 degrees flexion) during the application of the tape. Rotation of the knee should be avoided, which is best achieved by applying the tape on a standing patient with the leg to be taped on a 10-15 cm raised platform with the knee bent over the toes. Two anchors (A & B) are positioned approximately 10 cm over the joint line of the thigh and approximately 10 cm under the joint line of the lower leg respectively. These anchors should be open to the rear. A supporting tape (C) is applied from the anchor on the thigh, starting in the middle of the inner thigh and following the thigh length-wise downwards, continuing down to the lower leg. Because of the bend in the knee, the tape will be drawn to the front of the leg to be attached to the anchor. A supporting tape (D) is applied from the anchor on the lower leg, starting in the middle of the inner calf and following the leg length-wise upwards to the thigh. Due to the bend in the knee the tape will be drawn to the front of the thigh to be attached to the anchor. These two supporting strips now cross each other at the exact spot corresponding to the joint line, and consequently enables acceptable knee mobility. A third supporting tape can be applied between the two already in place. Finish with a further strip on top of each anchor A & B. |
ANKLE TAPE STIRRUP
Objective: Stabilise the ankle joint (talocrural and subtalar joints) against too great a lateral twist (supination and pronation) without reducing the normal mobility of the ankle joint (plantar and dorsal flexion). With a heavy sprain the applications include “stirrups”, “ankle lock” and possibly “figure-8”, however, light sprains normally require just “stirrups”. The tape is utilised the whole day in the beginning of the course, being gradually reduced over the following three months. The tape is finally only used in connection with particular loads where there is risk attached. |
|||
 |
|||
| Application: The foot should be kept in a neutral position when applying the tape, at an angle of 90 degrees from the lower leg. One or two tape anchors are applied around the lower leg 10-20 cm above the ankle joint (A), followed by application of three stirrups. The stirrups are started from the anchor on the inner side of the leg if it is the outer tendons that are injured (95%), and the other way around in the rare cases where it is the inner tendons that are damaged. The stirrups are taken under the heel and drawn up to the anchor on the outer side of the leg. When applying the stirrups the outer border of the foot is pushed slightly up, whilst at the same time pulling the border slightly up with the tape. A stirrup (B) is applied with the rear half of the outer ankle knuckle directly under the tape. A sloping stirrup (D) starts from the anchor on the front side of the leg slanting down over the lower leg over the front half of the inner ankle knuckle, under the foot and over the front half of the outer ankle knuckle, and slanting in over the leg up to the anchor. Finish with a further strip on top of the anchor A. |
ANKLE TAPE DOUBLE FIGURE-8 BANDAGE
Objective: Stabilise the ankle joint (talocrural and subtalar joints) against too great a lateral twist (supination and pronation) without reducing the normal mobility of the ankle joint (plantar and dorsal flexion). With a heavy sprain the applications include “stirrups”, “ankle lock” and possibly “figure-8”, however, light sprains normally require just “stirrups”. The tape is utilised the whole day in the beginning of the course, being gradually reduced over the following three months. The tape is finally only used in connection with particular loads where there is risk attached. Especially used with sprains of the tendon in the front of the ankle joint (lig. tibiofibular anterior), where pain is experienced when flexing the foot powerfully upwards (dorsal flexion). This tape must be rolled loosely on, and must not be drawn tight. If the tape becomes tight all the same, which often happens, it must be loosened. |
|||
 |
|||
| Application: Start at the back of the foot just in front of the ankle joint and draw the tape down around the outer border of the foot (A), under the sole and up to the back of the foot. Continue over the lower part of the ankle knuckle behind the heel under the Achilles tendon (B). The tape crosses down under the inner side of the heel and up to the outer border of the foot (C). The tape continues over the lower part of the inner ankle knuckle behind the heel under the Achilles tendon. The tape crosses the earlier tape, goes down under the outer side of the heel (D) and up to the inner border of the foot to finish on the back of the foot. |
ANKLE TAPE FIGURE-8 BANDAGE
Objective: Stabilise the ankle joint (talocrural and subtalar joints) against too great a lateral twist (supination and pronation) without reducing the normal mobility of the ankle joint (plantar and dorsal flexion). With a heavy sprain the applications include “stirrups”, “ankle lock” and possibly “figure-8”, however, light sprains normally require just “stirrups”. The tape is utilised the whole day in the beginning of the course, being gradually reduced over the following three months. The tape is finally only used in connection with particular loads where there is risk attached. |
|||
 |
|||
| Application: Begin just in front of the ankle joint and draw the tape in under the arch of the foot on the inner side, and up over the outer side, continuing over the start tape in front of the ankle joint and round behind the leg and back again to finish in front of the ankle joint. |
