


|
|
|
A precise diagnosis can be made in far the majority of cases from the case history and a clinical examination. In many cases it will, however, be advantageous to supplement with: |
|
X-ray, which is primarily used for suspicions of fractures and bone membrane tears (avulsion). The examination entails exposure to x-ray irradiation. |
|
CT-scanning, which is used with certain fractures as a supplement to ordinary x-ray examination. The examination entails marked exposure to x-ray irradiation. |
|
MRI-scanning, which is primarily indicated in cases where further examination of the conditions inside the joints is desired – since ultrasound scanning is easier, considerably cheaper and presumed just as effective in evaluating conditions outside of the joints. The examination entails exposure to magnetic irradiation, which is, as far as anyone knows, harmless. |
|
Diagnostic blockade with local anaesthetic has only modest risks associated with it if performed with the correct injection technique (possibly under guidance of ultrasound), and can contribute with considerable diagnostic information. |
|
Arthroscopy, which is used for diagnostic examination of the conditions in the joint if it is not possible to determine “from outside” what is wrong in the joint despite use of all other modern technology. This method is associated with a number of risks in relation to the other examination methods. |
|
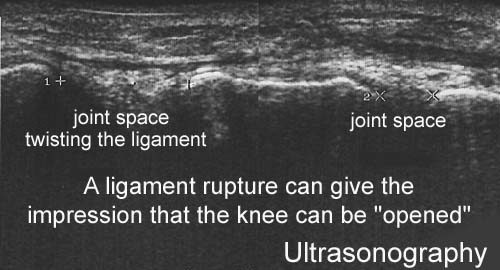
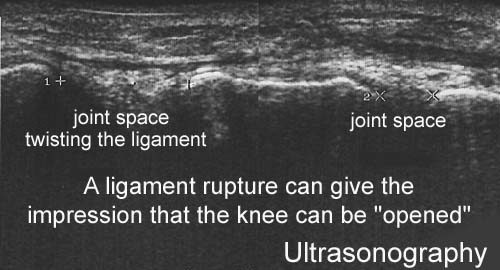
Ultrasound scanning, which is the cheapest, quickest and most suitable examination to enhance the findings from a clinical examination. The examination entails exposure to ultrasound irradiation which is completely harmless. |
|
Ultrasound scanning has developed rapidly over the recent decades. Ultrasound scanning is today an integral part of the clinical examination associated with sports medicine and other rheumatology related conditions, and acts as the physician’s “extended hand”. Ultrasound scanning will generally contribute to clarifying matters where the diagnosis is not certain, or the course of events is not as could be expected. Ultrasound scanning is particularly suitable for revealing the structures outside, and within the joints. The examination allows evaluation of the muscles, tendons and joints when activated (dynamic ultrasound scanning) (Ultrasonic image) as well as ultrasound-guided diagnostic and therapeutic draining of accumulations (blood, joint fluid, etc.). Furthermore, ultrasound-guided injection provides the possibility of placing the needle within a range of precision of 1/10 mm (Ultrasonic image). Injections which have earlier been performed “blind” have only been successfully placed at the desired location in under half of the attempts, and in more than 50% of the cases have erroneously hit other structures. It is for this reason that all injections where error in placement involves certain risks (injection around the large tendons and in the vicinity of large vessels and nerves) should always be performed under guidance of ultrasound. The correct placement of the needle can be performed by direct visualization of the tip of the needle in the most instances, but a small volume of sterile air (less than one drop) acts as an effective contrast medium and can ascertain a 100% correct placement of the needle in all injections, (article), (Ultrasonic image). Examples where ultrasound scanning has enabled precise diagnosis and treatment: |
| Case history 1: Stress fracture (Ultrasonic image) |
| Case history 2: Meniscus lesion, (Ultrasonic image)
Case history 3: Bursitis of the tendon of the knee (Baker’s cyst) (Ultrasonic image) |
| Case history 4: Injection, Jumper’s knee (Ultrasonic image), (Ultrasonic image), (Ultrasonic image).
Case history 5: Myositis ossificans, (Ultrasonic image) |
re. diagnosis. In the majority of cases, a precise diagnosis can be made based on the case history and a clinical examination. re. acute treatment. The aim of acute treatment is primarily to avoid further injury, and reduce the hemorrhaging as much as possible. re. medicinal treatment. Medicinal treatment is always merely a supplement to the primary treatment of sports injuries. re. inflammation. All injuries provoke an acute inflammation, which is crucial for the healing process of the injury. re. tape. Taping or bandaging is designed to relieve the injured structure by use of special tape attached externally. re. rehabilitation. A large number of sports injuries are caused by overload due to incorrect rehabilitation. re. complication of muscle ruptures. Calcification, scar tissue formation, blood accumulation or fluid development in the muscle, acute muscle compartment syndrome, chronic muscle compartment syndrome. |
SportNetDoc
| COMPLICATION OF MUSCLE RUPTURES IN GENERAL : |
|
| CORTICOSTEROIDER (binyrebarkhormon)
Injektion af binyrebarkhormon i sportsmedicin anvendes på følgende indikationer
Ingen anden lovlig behandling af idrætsskader har været så kontroversiel som lokal injektion af binyrebarkhormon. Der findes dog ikke i litteraturen dokumentation for, at injektion af binyrebarkhormon rundt om senerne, i led eller i slimsække skulle være skadelig. Injektioner direkte ind i senerne bør til gengæld frarådes, da enkelte dyreundersøgelser tyder på at senen svækkes. (article). Indikationer. Arthritis (hævelse af led på grund af “gigt”). Injektion i leddet af binyrebarkhormon er en af de mest anvendte behandlinger ved gigtsygdomme. Placebo kontrollerede undersøgelser har dokumenteret effekten af denne form for behandling. Virkningsmekanisme. Virkningsmekanismen er ikke fuldt afklaret. Bivirkninger. Infektionsrisikoen er yderst beskeden ved overholdelse af enkle sterile regler (afspritning minimum 2 gange, sterilt udstyr, “non-touch teknik”). Afblegning af huden over injektionen med synlige hudkar til følge, let ændret følsomhed på området samt delvis svind af fedtvævet er hyppigt forekommende, men giver kun gener i meget sjældne tilfælde. De fleste gener svinder spontant efter adskillige måneder (år). Risikoen for systemisk effekt efter injektion af binyrebarkhormon er mest teoretisk, skønt ansigtsblussen, menstruationsforstyrrelse, svingning i blodsukker og overfølsomhedsshock er beskrevet. Kontraindikationer. Mistanke om infektion i nærheden af injektionsstedet og aktiv tuberkulose. Der er kun beskeden erfaring med injektion af børn, hvorfor denne behandling yderst sjældent er indiceret hos børn. Administration. Binyrebarkhormonet blandes med lokalbedøvelse før injektionen. Herved nedsættes risikoen for bivirkninger og den midlertidige dæmpning af smerterne (pga lokalbedøvelsen) hjælper til at bekræfte (eller afkræfte) diagnosen. Diskussion. Injektion rundt om sener med binyrebarkhormon kan blandt andet bruges som supplement til behandling ved kroniske overbelastningsbetingede seneskader. Grundbehandlingen er “aktiv hvile” med stigende belastning inden for smertegrænsen. Hvis ikke idrætsudøveren følger genoptræningsreglerne og i stedet forcerer genoptræningen vil den kroniske “betændelse” (inflammation), den langvarige belastningspause og den pludseligt øgede træningsmængde medføre risiko for bristning af senen. Konklusion. Lokal injektion af binyrebarkhormon synes effektiv ved behandling af slimsæksbetændelser, senebetændelser, seneskedebetændelser, betændelse af vævet rundt om senerne og væskeansamling i leddene (traumatisk arthritis/synovitis) skønt den videnskabelige dokumentation er sparsom.
|
|
SIMPLE ANALGESIC. Indication. Analgesic drugs (painkillers) can be used to a limited extent to reduce the pain with minor injuries where there are no risks of aggravating the injury through continued sports activity (i.e. bleeding under the nail, skin abrasions etc.). All forms of painkillers can naturally be taken if the sports activity ceases. Paracetamol is recommended due to the very modest side effects associated with its use. Mechanism of action. Paracetamol provides both painkilling (analgesic) and temperature lowering (antipyretic) effects. The mechanism is partly unknown. 90% is absorbed from the intestines after ingestion of a tablet, with maximum concentration of paracetamol being achieved after ½-1 hour after ingestion. The duration of the effect is 4-6 hours. It should be noted that only approx. 60% is absorbed from suppositories. Side effects. Paracetamol in normal doses has by and large no side effects, as opposed to weak morphine type drugs containing acetyl salicylic acid. Long term treatment with maximum dosage appears, however, to increase the risk of ulcers, especially if the treatment is combined with rheumatic pills (NSAID), (article). Contraindications. Painkillers should never be used to enable the athlete to continue an activity which bears a risk of aggravating the injury. Paracetamol and other painkilling drugs with antipyretic effects must never be used to lower the body temperature of an athlete before starting sports activity. Serious virus infections can invade the (cardiac) muscle of the heart and cause myocarditis. The risk of myocarditis is increased under great physical exertion during virus infections, and some cases have been reported of fatalities amongst young, otherwise healthy athletes, under these circumstances. Increased body temperature indicates an infection, and all athletes should stop sports activity until the body temperature has returned to normal. Conclusion. Paracetamol can be recommended when needed as painkillers for conditions where pain is experienced without any suspicions of inflammation. |
| Instructions.
Rehabilitation begins with the exercises at Step-I. When the exercises at Step-I can be performed without pain (whilst performing the exercises, in the evening or next morning), the exercises at Step-II can be commenced. When the Step-II exercises can be completed without discomfort, the exercises at Step-III can be started, following on to Step-IV. If any soreness is experienced upon completion of the exercises which gives cause for any doubt as to whether this is due to normal muscle stiffness following training, or more of a “warning” soreness due to the intensity of the training increasing too quickly, the next training session should be performed on the same level. If the soreness subsequently diminishes, the soreness can be attributed to normal muscle stiffness, and the rehabilitation can be cautiously increased. If, on the other hand, the soreness does not decline, the rehabilitation is being forced too quickly, and the load has exceeded the limit which the injury is capable of managing for the time being. The training load and intensity should consequently be reduced immediately, and training should continue on a lower level for some days before being cautiously increased again. The amount of time which it is possible to use on the rehabilitation exercises naturally varies greatly from person to person, and the indications given should therefore be considered as a guideline for the relationship between strength, coordination and agility training, and can be amended according to the training opportunities which are available, as well as individual requirements. The rehabilitation period will generally pass quicker if more training is performed. However, if the guidelines in SportNetDoc go against information from your own doctor, you should naturally follow the advice of the doctor which has examined and evaluated your injury. The guidelines in Rehabilitation, general should be read before the exercises in Steps I-IV are commenced.
|
| REHABILITATION
In simple terms, sports injuries occur when the tissue is subjected to a load that exceeds the strength of the tissue. |
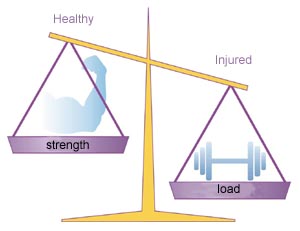 |
| The imbalance between the tissue strength (level of training) and the load is vital in understanding sports injuries – partly understanding how the injuries occur and partly how the injuries should be treated or prevented. The risk of the injury (re)occurring is therefore reduced not only by reducing the load or strain, but also by increasing the level of training.
This entails that the damaged tissue (muscle, tendon, ligament, bone) must be relieved, but also that a controlled training of the damaged tissue must be performed so that it becomes even stronger than before the injury occurred. The injured athlete must therefore train general fitness, strength and agility, as well as special training aimed at slowly increasing the strength of the damaged tissue. Injured athletes must therefore train even more than healthy athletes. In some cases the injury is a result of poor equipment (i.e. inferior running shoes), incorrect technique or inappropriate training (i.e. increasing the intensity of the training much too quickly). It is absolutely vital that these conditions are altered, as the injury will otherwise reappear relatively quickly after a training break due to injury. Many sports injuries are caused by over-load due to incorrect (re)training. Four weeks’ training is required in order to have any effect on muscle strength, four months to have an effect on bone strength, and eight months’ training to have any effect on tendon and ligament strength. Rapidly increasing intensity and quantity of training will therefore quickly increase the strength of the muscles, and consequently the load the muscles transfer to the tendons and bones. The tendons and bones are, however, not as yet fully trained to manage the increased load resulting in over-load symptoms from the bones (i.e. inflammation of the shin bone (shin-splint), stress fracture), or the tendons (i.e. inflammation of the Achilles tendon, groin, hollow foot tendon, knee cap tendon etc.). To guard against over-load injuries, the training quantity and intensity must be increased so slowly that the muscles, bones and tendons can all adjust to the increased load. When the tissue is damaged, this usually entails bleeding and release of fluid in the tissue thereby causing pain. Acute injuries can result in such heavy bleeding that swelling and pain quickly appear. Injuries from over-load usually entail such moderate bleeding and release of fluid in the tissue that tenderness often does not develop for the first few hours (appearing in the evening or next morning). This tenderness is however an important signal that the tissue has been subjected to a greater load than it is trained to manage, and that some damage has (re)occurred. It is often only necessary to undergo a few days’ relief and special training to make the symptoms disappear if training is immediately adjusted. If training is not adjusted the over-load will continue and the injury will, over the course of days to months, develop into a prolonged and in worst case chronic injury, which will render sports activity impossible for months or years. It is therefore absolutely vital that the athlete learns to listen to the body’s signals and adjusts training as soon as pain arises. All rehabilitation should be performed within the pain threshold. Rehabilitation of sports injuries is divided into two parts: Part 1 comprises relief of the damaged tissue (tendon, ligament or muscle) as long as there is swelling or pain in evidence. It is important to avoid total breaks in training, and training of all muscles and joints which are not injured should be continued. It takes much longer to build up tissue than to break it down, and it can therefore take several months to build up form again after “three weeks’ break”. All breaks in training weaken all muscles, tendons, ligaments and bones, which means that there is a considerable risk of incurring injury when training is commenced once again. Whilst the athlete is resting the damaged tissue, the following can by and large always be continued:
This type of relief is termed “ACTIVE REST”. Part 2 comprises a specific rehabilitation of the damaged tissue, with the aim of making the tissue so strong that it can manage the required load. To reduce the risk of a relapse of the injury it is necessary for the tissue to be even stronger than prior to the injury breaking out. The specific rehabilitation should be commenced 24-48 hours after the injury has occurred (so as not to risk the bleeding becoming worse). Medicinal treatment does not advance the course of Part 2 of the rehabilitation, as no legal substances will be able to increase the tissue’s strength. This can only be achieved through sensible training. |
 |
The knowledge we have today does not present a clear-cut picture of the connection between the occurrence of injuries in relation to training intensity, bodily stature and the development of puberty. As with adults, sports injuries in young athletes occur when the tissue is subjected to a load that exceeds the strength of the tissue
It is therefore vital that the warning signals that the body sends out (pain, tenderness, reduced ability, swelling) are treated with the proper respect. Over-load injuries in young athletes are often centred on the bone growth zone (apophysis), as well as the muscle and tendon attachments. Over-load injuries are especially seen during the period of rapid growth at the beginning of puberty. The acute injuries primarily comprise fractures, stress fractures, tears, dislocations and ligament injuries. It is especially important for children and adolescents to be medically examined at the slightest sign of injury, unless of course the injury is very commonplace or trivial. The fact that many longer-term illnesses often present themselves in children for the first time in connection with performing sports and games must also be taken into consideration. This can, for example, include forms of arthritis or other medicinal conditions that involve the “moving parts”. Infections or cysts in the muscles or bones are often first seen showing discreet symptoms whilst doing sport. Although these conditions are relatively rare, it is naturally vital for the treatment’s result that the conditions are diagnosed as early as possible so that the correct treatment can be started. It is of utmost importance that all rehabilitation for children and adolescents is performed within the pain threshold. Young athletes are very often not good at registering and reacting to the body’s warning signals and adjusting rehabilitation to follow these signals (tenderness, swelling, reduced ability), which will entail a higher risk of the rehabilitation following a “saw tooth” pattern with alternating progress and relapse, instead of a steady but slower progress. This is the classic sign that the warning signals are not observed and respected, and that the rehabilitation is being forced quicker than the injured tissue can manage. The social aspect associated with playing sport is of great importance for many children. It is therefore very important that rehabilitation exercises take place at the same time, and together with, the training of the team-mates who are not injured. It is always possible to prepare some rehabilitation exercises in one form or another which makes this achievable. It is therefore not optimal that “rehabilitation” consists of a total break from sport at home until the pain has gone before contacting the club to take part in normal training once again. All rehabilitation should therefore take place at the same location as the training for the team-mates that are not injured, and of course to the extent possible, the injured children should participate with the others in the normal training (i.e. warming up, light technical exercises, etc.). When the “normal” training involves exercises that the injured team mate can not take part in at the actual stage of his rehabilitation, the person injured can perform some special exercises, but in the same area as the others. The majority of sports injuries in children and adolescents can be treated with short-term relief, whilst other injuries will require a simple rehabilitation programme that can be found and downloaded from the children’s section of www.sportnetdoc.com. These exercises can in many cases be made more specific to the actual sport, and be amended so that they can be performed at the same place and at the same time as the non-injured team-mates. Some more serious injuries in children and adolescents will demand a more detailed and specialised rehabilitation program, which to a large extent can be found and downloaded from the adult section of www.sportnetdoc.com. It is important to point out that a standard rehabilitation program cannot be a substitute for a specific medical evaluation of the injury, and specific instruction.
|
| Instructions for rehabilitation.
Rehabilitation begins with the exercises at Step-I. When the exercises at Step-I can be performed without pain (whilst performing the exercises, in the evening or next morning), the exercises at Step-II can be commenced. When the Step-II exercises can be completed without discomfort, the exercises at Step-III can be started, following on to Step-IV. If any soreness is experienced upon completion of the exercises which gives cause for any doubt as to whether this is due to normal muscle stiffness following training, or more of a “warning” soreness due to the intensity of the training increasing too quickly, the next training session should be performed on the same level. If the soreness subsequently diminishes, the soreness can be attributed to normal muscle stiffness, and the rehabilitation can be cautiously increased. If, on the other hand, the soreness does not decline, the rehabilitation is being forced too quickly, and the load has exceeded the limit which the injury is capable of managing for the time being. The training load and intensity should consequently be reduced immediately, and training should continue on a lower level for some days before being cautiously increased again. The amount of time which it is possible to use on the rehabilitation exercises naturally varies greatly from person to person, and the indications given should therefore be considered as a guideline for the relationship between strength, coordination and agility training, and can be amended according to the training opportunities which are available, as well as individual requirements. The rehabilitation period will generally pass quicker if more training is performed. However, if the guidelines in SportNetDoc go against information from your own doctor, you should naturally follow the advice of the doctor which has examined and evaluated your injury. The guidelines in Rehabilitation of children and adolescents should be read before the exercises in Steps I-IV are commenced.
|