|
US of the painful hip in childhood: diagnostic value of cartilage thickening and muscle atrophy in the detection of Perthes disease. |

|
US of the painful hip in childhood: diagnostic value of cartilage thickening and muscle atrophy in the detection of Perthes disease. |
|
Secondhand smoke, hypofibrinolysis, and Legg-Perthes disease. Glueck CJ, Freiberg RA, Crawford A, Gruppo R, Roy D, Tracy T, Sieve-Smith L, Wang P. Clin Orthop 1998 Jul;(352):159-67 |
|
Osteonecrosis of the femoral head associated with slipped capital femoral epiphysis. Kennedy JG, Hresko MT, Kasser JR, Shrock KB, Zurakowski D, Waters PM, Millis MB. J Pediatr Orthop 2001 Mar-Apr;21(2):189-93 |
|
Slipped capital femoral epiphysis: evaluation of different modes of treatment. Rostoucher P, Bensahel H, Pennecot GF, Kaewpornsawan K, Mazda K. J Pediatr Orthop B 1996 Spring;5(2):96-101 |
|
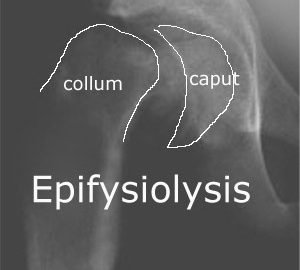
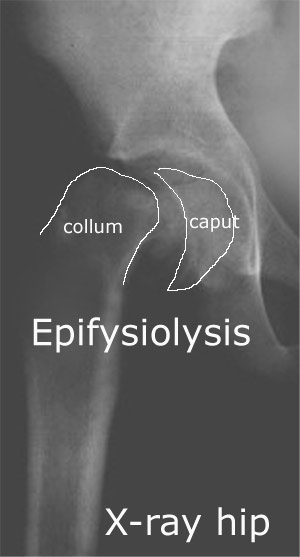
Diagnostic imaging of the early slipped capital femoral epiphysis. Magnano GM, Lucigrai G, De Filippi C, Castriota Scanderberg A, Pacciani E, Toma P. Radiol Med (Torino) 1998 Jan-Feb;95(1-2):16-20 |
|
Surgery for groin and lower abdominal pain in soccer players. |
|
Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. METHODS. RESULTS. CONCLUSIONS. |
|
Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. METHODS. RESULTS. CONCLUSIONS. |
|
Longstanding groin pain in athletes. A multidisciplinary approach. |