|
Anterior cruciate ligament injuries in the skeletally immature patient. |
Kategoriarkiv: Knee
treatment-article2
|
Anterior cruciate injuries in the skeletally immature athlete: a review of treatment outcomes. |
treatment-article1
|
ACL injuries in the skeletally immature patient.
|
examination-article1
|
Diagnosis of acute rupture of the anterior cruciate ligament of the knee by sonography. |

ultrasonic-image

Pivot shift
front drawer looseness
STEP1
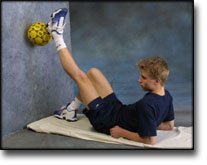
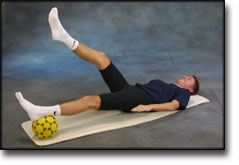
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR RUPTURE OF THE OUTER COLLATERAL LIGAMENT
(RUPTURA COLLATERALE LIGAMENTUM MEDIALE/TIBIALE)
STEP 1 |
Unlimited: Cycling with raised saddle.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
STEP2
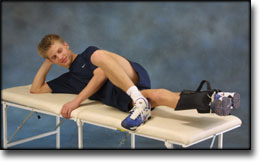
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR RUPTURE OF THE OUTER COLLATERAL LIGAMENT
(RUPTURA COLLATERALE LIGAMENTUM MEDIALE/TIBIALE)
STEP 2 |
Unlimited: Cycling. Swimming. Light jogging.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
STEP3
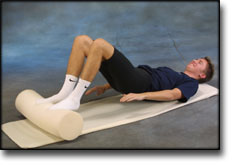
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR RUPTURE OF THE OUTER COLLATERAL LIGAMENT
(RUPTURA COLLATERALE LIGAMENTUM MEDIALE/TIBIALE)
STEP 3 |
Unlimited: Cycling. Swimming. Running with increasing speed and cautious directional change.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |