GENOPTRÆNING
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
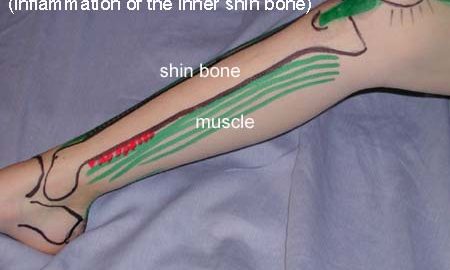
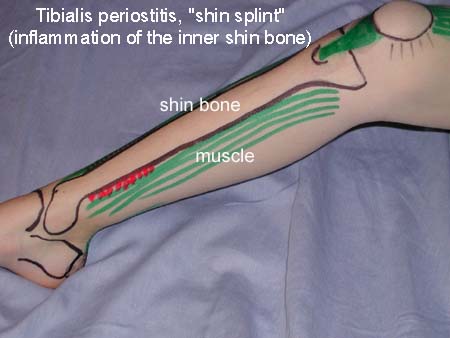
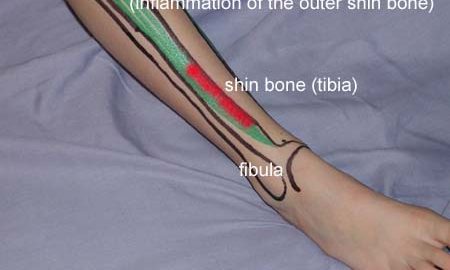
FOR INFLAMMATION OF THE INNER SHIN BONE
(MEDIAL TIBIAL PERIOSTITIS, “SHIN SPLINT”)
STEP 2 |
| The following rehabilitation program will cover the needs of the vast majority of children with inflammation of the inner shinbone. Older teenagers involved in sports at a high level can advantageously use the rehabilitation program for adults. | ||||||||||||||||||||||||||
Unlimited: Cycling. Swimming. Light jogging. (5 min)
|
||||||||||||||||||||||||||
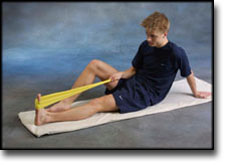
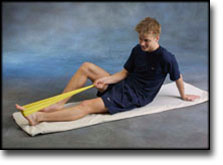
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |