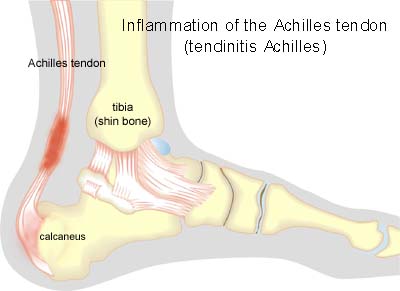
| Cause: Inflammation occurs with continued overload in the form of running and jumping. The risk of over-load injuries of the Achilles tendon increases with age.
Symptoms: Pain when activating the Achilles tendon (running and jumping), when applying pressure and with stretching of the tendon. The tendon often feels thickened.
Acute treatment: Click here.
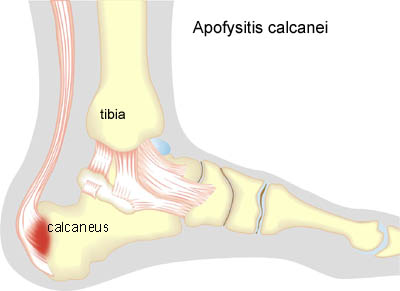
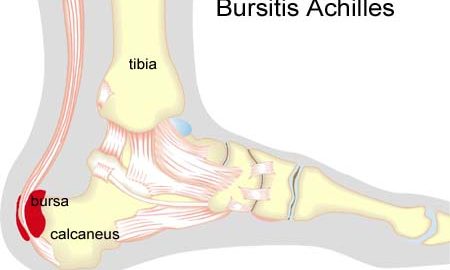
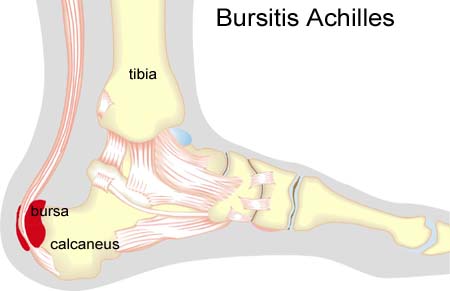
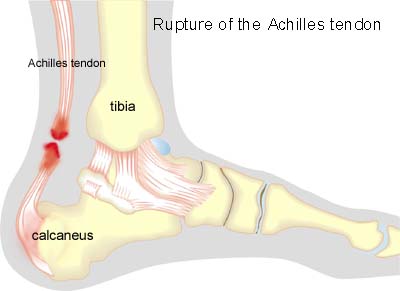
Examination: Medical examination is not necessarily required in slight, early cases where the tenderness is slowly increasing without sudden worsening. In cases when there is a sense of a “crack”, or sudden shooting pains in the Achilles tendon, medical attention should be sought as soon as possible to exclude a (partial) rupture of the Achilles tendon or rupture of the soleus muscle. This situation is best determined by use of ultrasound scanning, as a number of injuries requiring treatment can easily be overlooked during a normal clinical examination. In all cases where satisfactory progress is not in evidence, an ultrasound examination should be performed as early as possible. Ultrasound scanning enables an evaluation of the extent of the change in the tendon; inflammation of the tendon (tendinitis), development of cicatricial tissue (tendinosis), clacification, inflammation of the tissue surrounding the tendon (peritendinitis), inflammation of the bursa (bursitis), as well as (partial) rupture (article) (Ultrasonic image).
Treatment: Treatment is primarily comprised of relief from the painful activity (running). If the treatment is commenced early, the injury can in some cases heal within a few weeks. If the pain has been experienced for several months, and if ultrasound scanning has revealed thickening of, and changes in the tendon, a rehabilitation period of several months must be anticipated. Special emphasis is put on fitness training where the tendon is activated simultaneously with stretching (eccentric training) (article). It is naturally crucial that footwear is in good condition (good running shoes with shock absorbing heel and close fitting heel cap). Pressure on the Achilles tendon can be relieved by using shoes with an elevated heel, whilst a heel cushion in the shoe is of less significance since the heightening achieved by this method is greatly limited. If experiencing tenderness in the Achilles tendon during the rehabilitation period, treatment with ice for a period of at least 20 minutes is recommended. If the rehabilitation does not progress satisfactorily, medicinal treatment in the form of rheumatic medicine (NSAID) can be considered, or corticosteroid injection in the area surrounding the thickened part of the tendon. It is vital for safety that injections in the treatment of chronic Achilles tendon conditions are performed under ultrasound guidance. Studies have shown that ultrasound -guided injections of corticosteroid are extremely effective in reducing the extent of the thickened tendons, to enable more active rehabilitation to take place (article). As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or (further) rupture. The tendon is naturally unable to accommodate maximum strain or load after a prolonged injury period after only a short rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected (article). It is not unusual for a rehabilitation period of six months before maximum strain or load in the form of jumping is permitted. During recent years, different types of experimental treatment have been seen such as sclerosis injection (where injections are performed around the tendon with a drug to destroy the small blood vessels (and nerves) that infiltrate the sick tendons), and shock-wave (ultrasound treatment). However, there is no sure or clear documentation for the effect of these kinds of treatment. If satisfactory progress is not made in the rehabilitation and medicinal treatment, surgical intervention can be considered. Long-term results of operations are often disappointing (article-1), (article-2).
Bandage: Taping to relieve problems with the Achilles tendon is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction).
Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude:
Few sports injuries carry as large a risk of chronic, permanent sporting disability as inflammation of the Achilles tendon. In the severe, chronic cases, all treatment and rehabilitation attempts will often result in permanent inability to continue the sports activity.
Special: As inflammation of the Achilles tendon is extremely difficult to treat, it is important to prevent the injury from arising or recurring. The principles in (rehabilitation, general) should be followed to ensure that quickly increasing training loads at the season start, or after an injury period, are avoided. It is important that running shoes fit well (tight heel cap, shock absorbing soles). Ultrasound scanning of symptom-free athletes has shown changes in the tendon which increases the risk of developing symptoms during the next year. Preventive fitness and agility training (“Rehabilitation, specific”) can commence prior to the injury giving symptoms. It is therefore recommended that elite athletes over the age of 25 with high-load activities (running, jumping) have an ultrasound examination of the Achilles tendon once a year (article). In the event of unsatisfactory progress, or relapse after successful rehabilitation, consideration must be given to performing an analysis of the patient’s running style to establish whether a correction of the running style should be recommended. |