STRESS FRACTURE
|
||
|
||
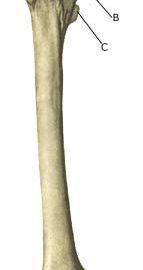
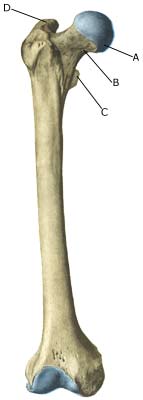
| Cause: Repeated loads, particularly when walking or running, can cause such great stress that cracks (stress fractures) appear in the shaft of the femur (article).
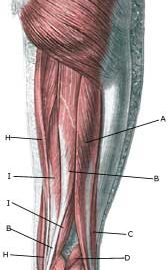
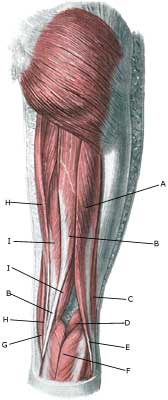
Symptoms: Pain and tired sensation in the thigh. The pain is aggravated upon applying pressure (direct and indirect tenderness) and applying load (walking, running). Examination: X-ray. Since many stress fractures are not visible early in the course, x-ray examination can be repeated after a few weeks, if stress fractures are still suspected. Scintigraphy, CT, MRI and ultrasound scans can often diagnose stress fractures far earlier than x-rays (Ultrasonic image). The frequency of stress fractures in the femur is probably more often than presumed (article). It is crucial for the result of the treatment that the diagnosis is made as early as possible (article). Treatment: The treatment primarily comprises relief. Only in special cases is surgery necessary (article). Rehabilitation: The rehabilitation is completely dependant on the type of fracture and the treatment (relief or surgical). A rehabilitation period of 2-4 months must be expected before maximum participation in sports activity can be resumed (article). Complications: If progress is not smooth, you should be medically re-evaluated to ensure that the fracture is healing according to plan. In some cases a false joint is formed (pseudoarthrosis), which requires surgical treatment. |