|
||
|
||
| Cause: When a muscle is subjected to a load beyond the strength of the muscle (jump, kick), a rupture occurs. The vast majority of ruptures are partial muscle ruptures. The weakest point is often at the junction between the muscle tendon and the muscle belly. Muscle ruptures in children and adolescents are relatively rare compared with adults.
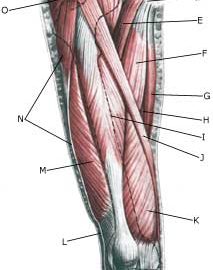
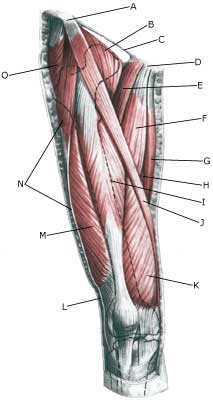
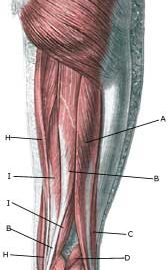
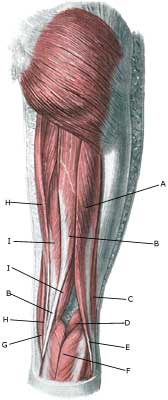
Symptoms: In slight cases a local tenderness is felt after being subjected to load (“sprained muscle”, “imminent pulled muscle”). In severe cases sudden shooting pains are felt in the muscle (“partial muscle rupture”, “pulled muscle”) and in the worst case a sudden snap is felt rendering the muscle unusable (“total muscle rupture”). The following three symptoms are characteristic in connection with muscle injuries: pain upon applying pressure, stretching and activation of the muscle (stretching knee) against resistance. With total ruptures a defect can often be seen and felt in the muscle, and above and below the rupture a swelling can be felt (the contracted muscle belly and bleeding). The most frequent place for partial ruptures on the anterior thigh is approximately 10 cm below the upper front iliac crest projection (spina iliaca anterior superior) in the rectus femoris muscle. Acute treatment: Click here. Examination: In very slight cases (light muscle sprains) with only minimal tenderness and no discomfort when walking normally, medical examination is not necessarily required. The severity of the tenderness is however, not always a measure of the extent of the injury. In cases of more pronounced tenderness or pain, medical examination is required to ensure the diagnosis and treatment. The diagnosis is usually made following normal medical examination, however, if there is any doubt concerning the diagnosis, ultrasound scanning can be performed, as it is the most suitable examination to ensure the diagnosis (Ultrasonic image). The larger the bleeding as assessed by ultrasound scanning, the longer the period needed to heal the injury (article). Treatment: The treatment of the vast majority of muscle injuries today involves relief and rehabilitation. It is only in very rare cases that surgery is indicated (e.g. total rupture in the anterior muscle tendon close to the attachment on the upper knee cap where surgery is recommended very quickly (article). Even large ruptures in the thigh muscles will usually be able to be healed and rehabilitated without giving functional disorder (but often cosmetic disfigurement with an irregular thigh muscle). Complications: If steady progress is not experienced, you should be medically (re)examined to ensure that the diagnosis is correct or whether complications for muscle ruptures have arisen. |