|
Local corticosteroid injection in sport: review of literature and guidelines for treatment. |
Kategoriarkiv: Inflammation of Achilles tendon
special-article
|
Significance of ultrasonographically detected asymptomatic tendinosis in the patellar and achilles tendons of elite soccer players: a longitudinal study. |
treatment-article2
|
Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. |
treatment-article1
|
Chronic Achilles tendinosis: recommendations for treatment and prevention. |
treatment-article4
|
Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper’s knee and Achilles tendinitis: a randomized, double-blind, placebo-controlled study. |
step4
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON
(TENDINITIS ACHILII)
STEP 4 |
Unlimited: Cycling. Swimming. Running with increasing distance on a soft surface.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
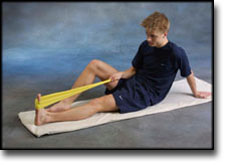
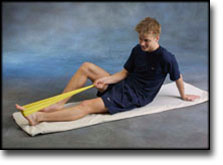
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step3
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON
(TENDINITIS ACHILII)
STEP 3 |
Unlimited: Cycling. Swimming. Light jogging on a soft surface.
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step2
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON
(TENDINITIS ACHILII)
STEP 2 |
Unlimited: Cycling. Swimming. Running in deep water.
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step1
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON
(TENDINITIS ACHILII)
STEP 1 |
| The indications of time after stretching, coordination training and strength training show the division of time for the respective type of training when training for a period of one hour. The time indications are therefore not a definition of the daily training needs, as the daily training is determined on an individual basis.
|
||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |