|
Interventions for preventing ankle ligament injuries.
Quinn K, Parker P, de Bie R, Rowe B, Handoll H. Cochrane Database Syst Rev 2000;(2):CD000018.
BACKGROUND.
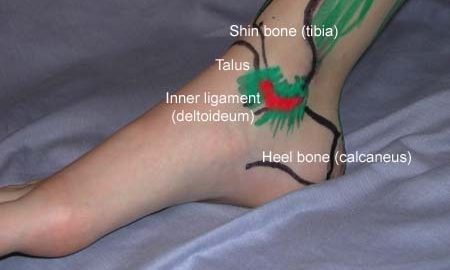
Some sports, for example basketball and soccer, have a very high incidence of ankle injuries, mainly sprains. This contributes to ankle sprains being one of the most commonly treated injuries.
OBJECTIVES.
To assess the effects of interventions used for the prevention of ankle ligament injuries or sprains in physically active individuals from adolescence to middle age.
SEARCH STRATEGY.
We searched the Cochrane Musculoskeletal Injuries Group trials register, MEDLINE (1966 to July 1996), EMBASE (1980 to September 1996), CINAHL (1982 to June 1996), and bibliographies of study reports. We also contacted colleagues and some trialists. Date of the most recent search: March 1997. S
ELECTION CRITERIA.
Randomised or quasi-randomised trials of interventions for the prevention of ankle sprains in physically active individuals from adolescence to middle age were included provided ankle sprains were recorded. Interventions include use of modified footwear and associated supports, adapted training programmes and health education.
DATA COLLECTION AND ANALYSIS.
At least four reviewers independently assessed methodological quality and extracted data. Wherever possible, results of outcome measures were pooled and sub-grouped by history of previous sprain.
MAIN RESULTS.
Five randomised trials with data for 3954 participants were included. All trials involved young, active, mostly male adults participating in high-risk, usually sporting, activities. With the exception of ankle disc training, all prophylactic interventions entailed the application of an external ankle support in the form of a semi-rigid orthosis, air-cast brace or high top shoes. There was a significant reduction in the number of ankle sprains in people allocated external ankle support (Peto odds ratio 0.49; 95% confidence interval 0.37 to 0.66). This reduction was greater for those with a previous history of ankle sprain, but still possible for those without prior sprain. There was no apparent difference in the degree of severity of the ankle sprain prevented nor any change to the incidence of other leg injuries. The protective effect of ‘high-top’ shoes remains to be established. There was limited evidence for reduction in ankle sprain for those with previous ankle sprains who did ankle disc training exercises.
REVIEWER’S CONCLUSIONS.
This review provides good evidence for the beneficial effect of ankle supports in the form of semi-rigid orthoses or air-cast braces to prevent ankle sprain during high-risk sporting activities (e.g. soccer, basketball). Participants with a history of previous sprain can be advised that wearing such supports may reduce the risk of incurring a future sprain. However, any potential prophylactic effect should be balanced against the baseline risk of the activity, the supply and cost of the particular device, and for some, the possible or perceived loss of performance. Further research is indicated principally to investigate other prophylactic interventions and general applicability.
|