|
Acute and chronic patella dislocations. Therapeutic strategies in Danish orthopedic departments. METHODS. RESULTS. CONCLUSION. |
Kategoriarkiv: Knee
examination-article1
|
Subluxation of the patella: evaluation of patellar articular cartilage with MR imaging. |
meniscus test
STEP4
Training ladder for:
MENISCUS LESION
(LAESIO TRAUMATICA MENISCI)
STEP 4 |
|
|||||||||||||||||||||||||||||||||||||
STEP3
Training ladder for:
MENISCUS LESION
(LAESIO TRAUMATICA MENISCI)
STEP 3 |
|
|||||||||||||||||||||||||||||||||||||
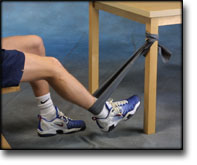
STEP2
Training ladder for:
MENISCUS LESION
(LAESIO TRAUMATICA MENISCI)
STEP 2 |
|
||||||||||||||||||||||||||||||||||
STEP1
Training ladder for:
MENISCUS LESION
(LAESIO TRAUMATICA MENISCI)
STEP 1 |
|
treatment-article2
|
Meniscal injury in children: long-term results after meniscectomy.
|
treatment-article1
|
Treatment of intrasubstance meniscal lesions: a randomized prospective study of four different methods. |
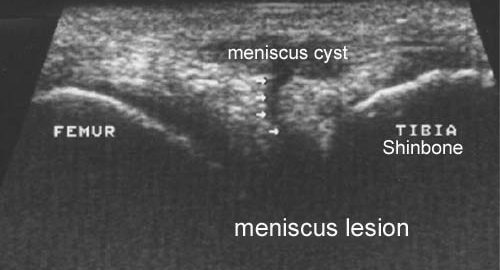
ultrasonic-image