|
Herniated cervical intervertebralp discs with radiculopathy: an outcome study of conservatively or surgically treated patients. |
Kategoriarkiv: Nerve entrapment on the back of the shoulder blade

Slipped disc in the neck
|
||
|
||
| Cause: If the neck is subjected to a load which exceeds its capabilities, a crack in one of the discs may occur so that the liquid content in the centre of the disc (nucleus pulposus) can be squeezed out and apply pressure on a nerve root.
Symptoms: Pain and stiffness in the neck, radiating to one of the arms. There can be sensory interference and reduction in arm strength. Symptoms are often aggravated by coughing. Examination: If a slipped disc is suspected medical attention should be sought at once so that special examinations can be performed (extent of sensory interference, reduction of muscle strength, reflexes, foramen compression test) to establish the diagnosis and which treatment should be initiated. In some cases it is necessary to supplement with an MRI scan if the treatment does not progress smoothly. Treatment: If examination reveals signs of a slipped disc without alarming symptoms (substantial deterioration of muscle strength/paralysis), treatment will primarily be directed at altering the imbalance between the load the neck is subjected to, opposed to the level the neck is trained to manage. It is therefore recommended that you are instructed (possibly by a physiotherapist) in the appropriate way to put a strain on the neck, and which loads and movements should be avoided (“ergotherapeutic guidance”). A few days’ rest and relief may be needed to subdue the pain, after which steadily increasing training should be started with neck and throat muscle exercises. If painkillers are required, paracetamol can be recommended, possibly combined with rheumatic medicine (NSAID). By far the majority of slipped discs can be managed through correct training. In cases where the above treatment does not produce progress in the condition, an MRI scan will be considered with a view to possible operation. Operation is therefore first considered if the rehabilitation programme does not succeed (article), and if the MRI scan can detect a prolapse which can explain the symptoms. In cases with alarming symptoms (substantial deterioration of muscle strength/paralysis) acute hospitalisation is recommended for evaluation of the need for acute surgery. Special: Training should be performed on a “lifelong” basis to reduce the risk of relapse after a successful rehabilitation. Smoking causes increased risk of pain by reducing the flow of blood to the cartilage discs (disci), implying that daily small injuries do not heal so well. Stopping smoking is therefore an important part of the treatment. |
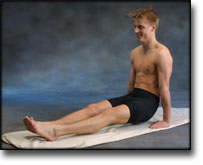
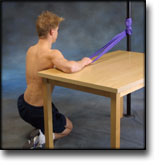
step4
Training ladder for:
NERVE ENTRAPMENT ON THE BACK OF THE SHOULDER BLADE
(ENTRAPMENT N SUPRASCAPULARIS)
STEP 4 |
Unlimited: Cycling. Swimming. Running.
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
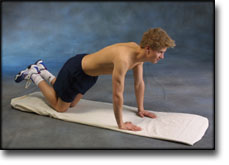
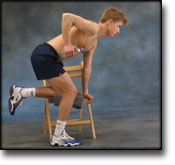
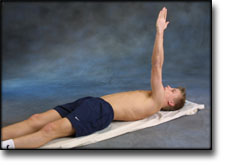
step3
Training ladder for:
NERVE ENTRAPMENT ON THE BACK OF THE SHOULDER BLADE
(ENTRAPMENT N SUPRASCAPULARIS)
STEP 3 |
Unlimited: Cycling. Swimming. Running.
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
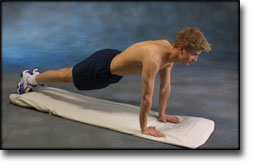
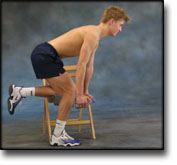
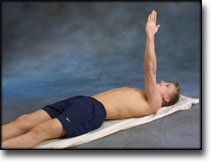
step2
Training ladder for:
NERVE ENTRAPMENT ON THE BACK OF THE SHOULDER BLADE
(ENTRAPMENT N SUPRASCAPULARIS)
STEP 2 |
Unlimited: Cycling. Swimming. Running.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
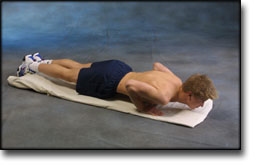
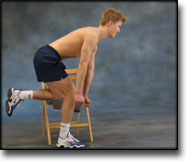
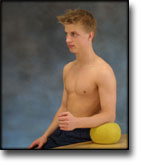
step1
Training ladder for:
NERVE ENTRAPMENT ON THE BACK OF THE SHOULDER BLADE
(ENTRAPMENT N SUPRASCAPULARIS)
STEP 1 |
| The indications of time after stretching, coordination training and strength training show the division of time for the respective type of training when training for a period of one hour. The time indications are therefore not a definition of the daily training needs, as the daily training is determined on an individual basis.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
treatment-article2
|
Scapular pain and supra-scapular neuropathy in sports medicine. |
treatment-article1
|
Entrapment of the suprascapular nerve. |
cause-article
|
Suprascapular neuropathy in volleyball players. METHODS. RESULTS. CONCLUSIONS. |