|
||
|
||
|
||
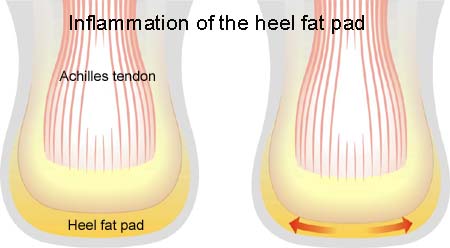
| Cause: Inflammation of the heel pad occurs often after repeated, vigorous, overload (for example landing after jumping). The injury is often seen in gymnasts.
Symptoms: Pain when walking as well as when applying pressure on the edges of the heel pad. In some cases, it will be possible to see haemorrhaging in the heel pad (article). Acute treatment: Click here. Examination: Medical examination is not always necessary in light cases with minimal tenderness and no pain when walking. If satisfactory progress is not made, or if there is a sense of a “snap”, or sudden shooting pains, medical attention should be sought as soon as possible to make the diagnosis. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis an ultrasound scan can be performed. Treatment: Rest from the painful activity (running). The injury can in some cases heal within a few weeks if treatment is commenced at an early stage. It is imperative that footwear is in order, with a suitably tight heel cap to hold the heel pad in place under the heel, and with shock absorbing soles. Rehabilitation: Treatment is primarily rest. The principles under rehabilitation, general can be followed until the pain has gone, after which running and jumping can be cautiously resumed. Bandage: Taping to relieve problems with inflammation of the heel pad is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction). Complications: If there is not a steady improvement in the condition, x-ray or an ultrasound scan should be performed to exclude:
Shock absorbing shoes or inlays will reduce the risk of inflammation of the heel pad. |