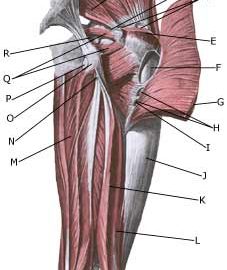
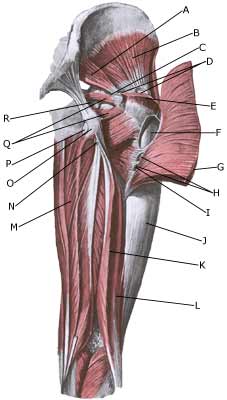
BURSITIS AT THE OUTER FEMORAL BONE PROJECTION
|
||
|
||
| Cause: In case of repeated loads or blows the bursa can become inflamed, produce fluid, swell and become painful.
Symptoms: Pain when applying pressure on the thigh corresponding to the bursa, which sometimes (but far from always) can feel swollen. The pain can radiate down the thigh. Acute treatment: Click here. Examination: In light cases with only minimal tenderness medical examination is not necessarily required. In case of more pronounced pain or lack of progress, a medical examination should be carried out to ensure the diagnosis and commencement of any treatment. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis an ultrasound scan can be performed (Ultrasonic image). Treatment: The treatment primarily comprises relief. If the direct cause of the complaint is known, it should of course be removed. The treatment can be supplemented with rheumatic medicine (NSAID) or injection of corticosteroid in the bursa, which is best performed under the guidance of ultrasound. Complications: If progress is not smooth, the correctness of the diagnosis should be considered or whether complications have arisen:
Special: Shock absorbing shoes or inlays will reduce the load. In case of lack of progress or recurrences after successful rehabilitation it can be considered to have a running style analysis, to evaluate whether correction of the running style is indicated. |