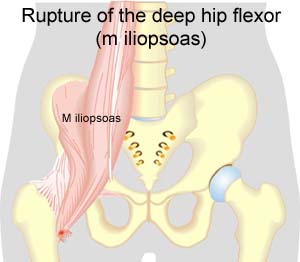
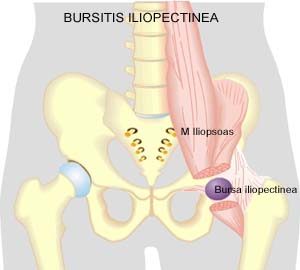
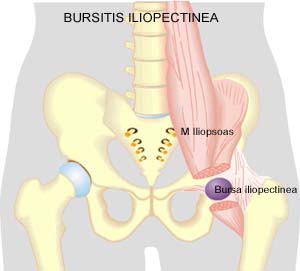
| Cause: When a muscle is subjected to loads (repeated smaller loads or one very powerful load), beyond the strength of the muscle (jumping, kicking), a rupture occurs. The rupture can be microscopic and due to repeated loads in continuing sports activity, many small loads can trigger a chronic inflammation or a rupture. The vast majority of cases are partial muscle ruptures.
Symptoms: In light cases a local tenderness is felt after the load (“muscle strain”, “imminent pulled muscle”, “tendinitis”). The symptoms can often decrease after a thorough warm-up, only to return when the sports activity has ceased. In severe cases a sudden shooting pain is felt in the muscle (“partial muscle rupture”, “pulled muscle”) and in the worst case a sudden snap is felt rendering the muscle unusable (“total muscle rupture”). With muscle injuries the following three symptoms are characteristic: pain when applying pressure, stretching and activation against resistance. In total ruptures a defect in the muscle can often be seen and felt, and a swelling is felt above or below the rupture (the contracted muscular belly and the bleeding).
Acute treatment: Click here.
Examination: In light cases with only minimal tenderness and no discomfort with ordinary walking, medical examination is not necessarily required. The extent of the tenderness is, however, not always a mark of the degree of the injury. In cases of more pronounced pain or tenderness, medical examination is required to ensure the correct diagnosis and treatment. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis an ultrasound scan can be performed (Ultrasonic image). X-ray examination is recommended when it is suspected that the bone on which the muscle tendon fastens has been torn off.
Treatment: The treatment usually comprises relief and rehabilitation. Only in very rare cases is surgery indicated (e.g. total ruptures in the muscle tendon, close to the fastening). Even large ruptures in the femoral muscle can usually be rehabilitated without resulting in functional harm (but often cosmetic damage, with an irregular femoral muscle). If the condition concerns tendinitis where there has been no sensation of a “snap” in the muscle, and smooth improvement has not been achieved after relief and gradually increasing rehabilitation, treatment can be supplemented with rheumatic medicine (NSAID) oand possibly injection of corticosteroid in the area surrounding the inflamed part of the muscle attachment point. If it concerns ruptures, (“total or partial muscle rupture”) the injection of corticosteroid is not indicated.
Complications: If the treatment does not progress according to plan, it should be considered whether the diagnosis is correct or whether complication have arisen. In particular the following should be considered:
|