|
||
|
||
|
||
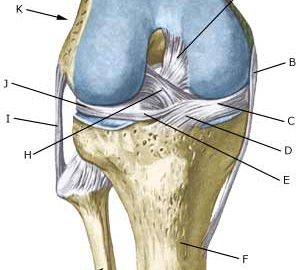
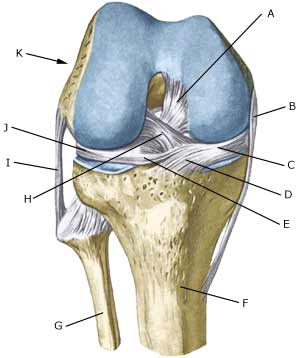
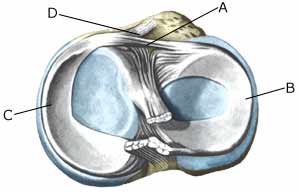
| Cause: Meniscus lesions often occur when the knee is stretched at the same time as rotating. The meniscus will consequently be squeezed between the thigh bone and the shin bone. The inner meniscus is more often damaged than the external. Meniscus injuries in children is very rare (article).
Symptoms: Pain along the joint line when applying pressure and when rotating the knee. The pain often occurs suddenly when performing certain movements, and can be accompanied by swelling of the knee. In some instances the knee can lock due to a splinter from the meniscus becoming jammed. In other cases, a small and tender outpouching of fluid can be sensed at the joint line (meniscus cyst). Prolonged discomfort will often cause the thigh muscle to diminish. Acute treatment: Click here. Examination: A medical examination is always necessary if there is any suspicion of injury within the knee joint. A normal clinical examination is often not sufficient. The doctor can perform various knee tests (meniscus test), however, there is typically tenderness along the joint line which is aggravated when rotating the knee joint. It is often necessary to perform an arthroscopy (telescopic examination of the joint), MR-scan or ultrasound scan to make the diagnosis (article) (Ultrasonic image). Treatment: In uncertain cases the treatment comprises relief and rehabilitation of the knee. If the discomfort does not slowly diminish, if there are instances of “locking” or if it is clear that the meniscus lesion is large (e.g. assessed from an ultrasound scan), surgery should be considered. Under an operation, it can be attempted to sew the torn piece of meniscus back (which will require a considerably longer rehabilitation period, but will probably in the long term reduce the risk of degenerative arthritis in the knee) (article). The torn piece of meniscus is usually removed, but in rare cases the whole meniscus is taken out. Following an operation, exerting load on the knee can commence as soon as the pain and swelling in the knee has diminished. In the best cases, full activity is possible after a period of a few weeks. In uncomplicated cases, it should be possible to resume a full level of sports activity during the course of a month. Rehabilitation must not be allowed to cause increased swelling (or pain) in the knee. Complications: If insufficient progress is made prior to an operation it must be considered if the diagnosis is correct. Supplementary examinations will often be required (X-ray, ultrasound or MR scan). In particular the following should be considered:
Following an arthroscopy, fluid accumulation in the joint (traumatic arthritis/synovitis) should be considered, and infection in the scar or knee joint, which will always require medical attention as soon as possible. Special: Since there is a risk that the injury can cause permanent disability, the injury should be reported to your insurance company. |