|
Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. |
Alle indlæg af urtehave_com
treatment-article1
|
Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional achilles tendinosis with calcific spur. |
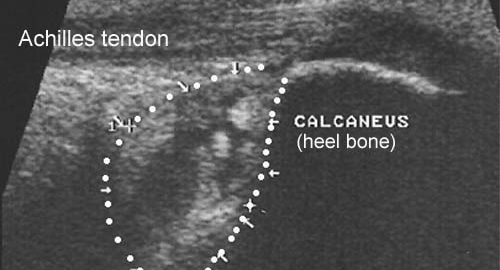
ultrasonic-image

step4
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON ATTACHMENT
(Achilles enthesopathy)
STEP 4 |
Unlimited: Cycling. Swimming. Running with increasing distance on a soft surface.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step3
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON ATTACHMENT
(Achilles enthesopathy)
STEP 3 |
Unlimited: Cycling. Swimming. Light jogging on a soft surface.
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step2
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON ATTACHMENT
(Achilles enthesopathy)
STEP 2 |
Unlimited: Cycling. Swimming. Running in deep water.
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
step1
Training ladder for:
INFLAMMATION OF THE ACHILLES TENDON ATTACHMENT
(Achilles enthesopathy)
STEP 1 |
| The indications of time after stretching, coordination training and strength training show the division of time for the respective type of training when training for a period of one hour. The time indications are therefore not a definition of the daily training needs, as the daily training is determined on an individual basis.
|
||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
treatment-article1
|
Chronic Achilles tendon pain treated with eccentric calf-muscle training. |
treatment-article2
|
Local corticosteroid injection in sport: review of literature and guidelines for treatment. |
treatment-article3
|
Local corticosteroid injection in sport: review of literature and guidelines for treatment. |