|
Acute elbow dislocation: evaluation and management. |
Alle indlæg af urtehave_com
treatment-article2
|
Return to Australian rules football after acute elbow dislocation: |
treatment-article1
|
Indications for operation in elbow dislocation. |
examination-article
|
Sonography compared with radiography in revealing acute rib fracture. |
cause-article
|
Stress fractures of the ribs in golfers. |
morphine type drugs
| WEAK MORPHINE TYPE DRUGS
Indication. Analgesic (pain killing tablets) can be used on a greatly limited scale to reduce pain in connection with minor injuries where this is a risk of aggravating the injury with continued activity (i.e. bleeding under the nail and the like). The treatment can naturally also be utilized in many other cases with pain present if the sports activity is discontinued (fracture, lumbago and the like). Mechanism of action. Weak morphines are pain killing tablets with a weak morphine-like effect. The effect is not substantially different from paracetamol. There are several different drugs within the “weak morphines” group, which are all absorbed via the intestines. The effect can be expected after approx. ½-1 hour, with a duration of 3-6 hours. Side effects. The side effects are of the same character (although weaker) as morphine: nausea, vomiting, drowsiness, constipation and dizziness, and therefore extreme caution should be exercised when driving. The drugs present only a limited risk of dependence and addiction. Overdoses can be life threatening. Contraindication. Pain killers should never be used to allow an athlete continue a sports activity which can bring about a risk of aggravating the injury. As there are different contraindications with all the drugs in the “weak morphines” group, the attending doctor should acquire a good knowledge of the patient before prescribing drugs from this group. Dose. Dependent upon which drug is used in the treatment. Conclusion. Weak morphines are almost never indicated in the treatment of sports injuries, as it is possible to achieve almost the same result with non-prescription drugs with considerably less risk attached. |

ultrasonic-image

step4
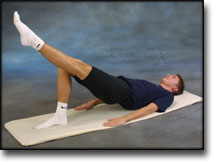
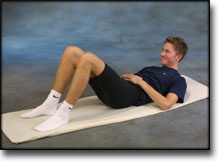
Training ladder for:
FRACTURE OF THE VERTEBRAL ARCH
(spondylolysis)
STEP 4 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
step3
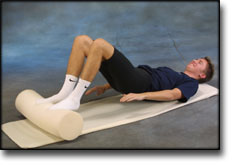
Training ladder for:
FRACTURE OF THE VERTEBRAL ARCH
(spondylolysis)
STEP 3 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
step2
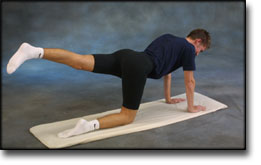
Training ladder for:
FRACTURE OF THE VERTEBRAL ARCH
(spondylolysis)
STEP 2 |
|
|||||||||||||||||||||||||||||||||||||||||||||