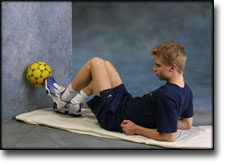
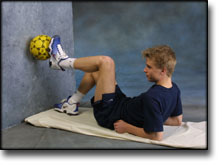
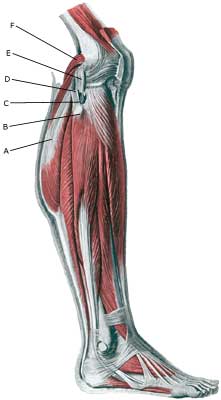
| Cause: When the shin bone is pressed inwards in relation to the thigh bone the outer side-ligament is stretched. If the load becomes sufficiently powerful (as is the case when the load is sudden, so that the thigh muscles do not have time to tighten and stabilize the joint) the ligament can rupture.
Symptoms: Sudden pain on the outside of the knee. Occasionally a snap is felt when the ligament ruptures. In severe cases the athlete complains about a sense of looseness in the knee.
Acute treatment: Click here.
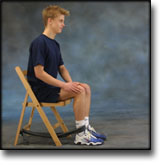
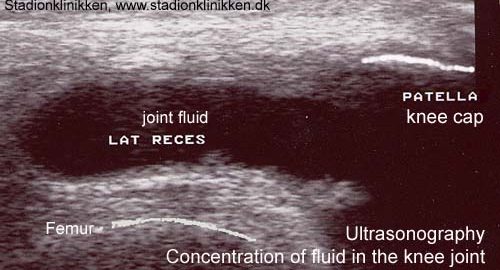
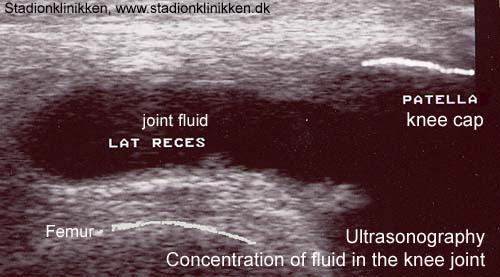
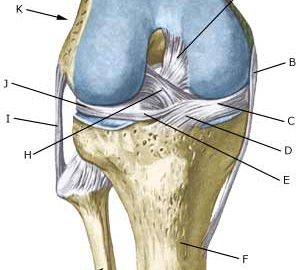
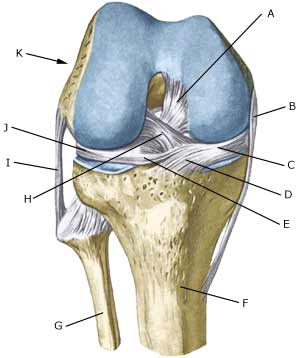
Examination: If a total or partial rupture of the ligaments in the knee is suspected, you should seek medical attention for a diagnosis. The doctor can perform various knee tests to examine the stability of the knee (external side-instability-test) . If the knee is stable the injury is called a “sprain” of the outer side-ligament. If the knee is loose the injury is called a “rupture” of the ligament. The diagnosis is usually made from a normal medical examination. If there are any doubts surrounding the diagnosis, an ultrasound scan can be performed which will reveal the rupture and the bleeding along the ligaments (Ultrasonic image).
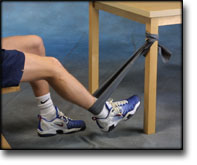
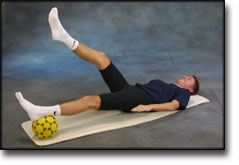
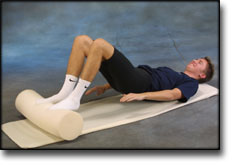
Treatment: The treatment of a partial or total rupture of the outer side-ligament involves relief and rehabilitation. If the knee is markedly loose, you can, for a short period, use a support splint (Don Joy). With pronounced sideways looseness surgery can be considered (article). (However if the rupture of the outer side-ligament is combined with other ligament ruptures, as is often the case, surgery is recommended).
Bandage: Hinge bandages can be used initially (Don Joy). Tape treatment of ligament ruptures in the knee have no sure effect.
Complications: If smooth progress is not achieved, it should be considered whether the diagnosis is correct or whether complications have arisen. Supplementary examinations (X-ray, ultrasound, MR scan or arthroscopy) will often be required. The following should be considered:
An inflammation by the ligament fastening is sometimes seen later in the course of the injury, and in some cases bursitis at the ligament fastening is seen. The inflammation and bursitis can possibly be treated with medication (rheumatic medicine (NSAID) or the injection of corticosteroid), if further relief has no effect (article).
Special: Since there is a risk that the injury can cause permanent disability, the injury should be reported to your insurance company. |