| CORTICOSTEROIDER (binyrebarkhormon)
Injektion af binyrebarkhormon i sportsmedicin anvendes på følgende indikationer
Ingen anden lovlig behandling af idrætsskader har været så kontroversiel som lokal injektion af binyrebarkhormon. Der findes dog ikke i litteraturen dokumentation for, at injektion af binyrebarkhormon rundt om senerne, i led eller i slimsække skulle være skadelig. Injektioner direkte ind i senerne bør til gengæld frarådes, da enkelte dyreundersøgelser tyder på at senen svækkes. (article). Indikationer. Arthritis (hævelse af led på grund af “gigt”). Injektion i leddet af binyrebarkhormon er en af de mest anvendte behandlinger ved gigtsygdomme. Placebo kontrollerede undersøgelser har dokumenteret effekten af denne form for behandling. Virkningsmekanisme. Virkningsmekanismen er ikke fuldt afklaret. Bivirkninger. Infektionsrisikoen er yderst beskeden ved overholdelse af enkle sterile regler (afspritning minimum 2 gange, sterilt udstyr, “non-touch teknik”). Afblegning af huden over injektionen med synlige hudkar til følge, let ændret følsomhed på området samt delvis svind af fedtvævet er hyppigt forekommende, men giver kun gener i meget sjældne tilfælde. De fleste gener svinder spontant efter adskillige måneder (år). Risikoen for systemisk effekt efter injektion af binyrebarkhormon er mest teoretisk, skønt ansigtsblussen, menstruationsforstyrrelse, svingning i blodsukker og overfølsomhedsshock er beskrevet. Kontraindikationer. Mistanke om infektion i nærheden af injektionsstedet og aktiv tuberkulose. Der er kun beskeden erfaring med injektion af børn, hvorfor denne behandling yderst sjældent er indiceret hos børn. Administration. Binyrebarkhormonet blandes med lokalbedøvelse før injektionen. Herved nedsættes risikoen for bivirkninger og den midlertidige dæmpning af smerterne (pga lokalbedøvelsen) hjælper til at bekræfte (eller afkræfte) diagnosen. Diskussion. Injektion rundt om sener med binyrebarkhormon kan blandt andet bruges som supplement til behandling ved kroniske overbelastningsbetingede seneskader. Grundbehandlingen er “aktiv hvile” med stigende belastning inden for smertegrænsen. Hvis ikke idrætsudøveren følger genoptræningsreglerne og i stedet forcerer genoptræningen vil den kroniske “betændelse” (inflammation), den langvarige belastningspause og den pludseligt øgede træningsmængde medføre risiko for bristning af senen. Konklusion. Lokal injektion af binyrebarkhormon synes effektiv ved behandling af slimsæksbetændelser, senebetændelser, seneskedebetændelser, betændelse af vævet rundt om senerne og væskeansamling i leddene (traumatisk arthritis/synovitis) skønt den videnskabelige dokumentation er sparsom.
|
Alle indlæg af urtehave_com
treatment-article2
|
Osteochondritis dissecans of the knee. |
treatment-article1
|
Treatment algorithm for osteochondral injuries of the knee.
|
treatment-article
|
Osteochondral injuries. Clinical findings. |
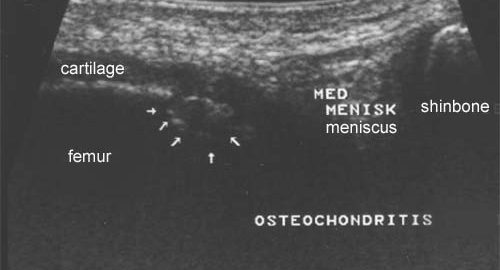
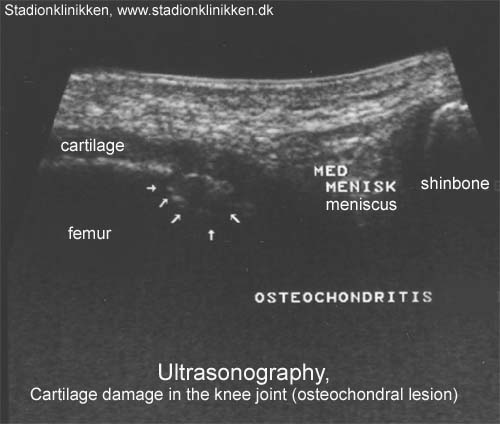
ultrasonic-image
examination-article3
comming soon
examination-article2
|
Osteochondritis dissecans of the knee in children. A comparison of MRI and arthroscopic findings. |
examination-article1
|
Arthroscopic versus conservative treatment of osteochondritis dissecans of the knee: value of magnetic resonance imaging in therapy planning and follow-up. |

photo

week15+
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR RUPTURE OF THE POSTERIOR CRUCIATE LIGAMENT
(RUPTURA LIGAMENTUM CRUCIATUM POSTERIUS)
WEEK 15 + |
| The following exercises can only be considered as a supplement to the guidelines furnished by the doctor which performed the operation. Specific precautions are necessary as the operation can be complicated. The training must not bring about swelling or pain in the knee. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unlimited: Cycling. Swimming. Running.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
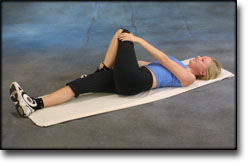
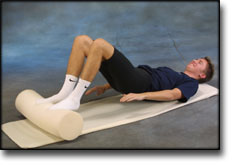
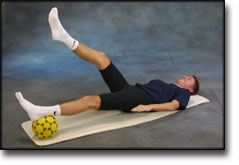
| Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated.
The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |