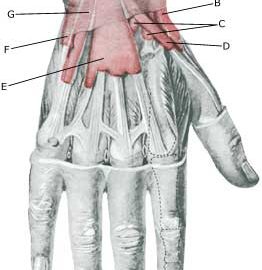
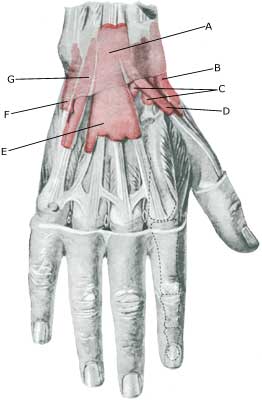
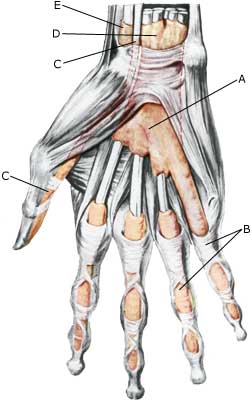
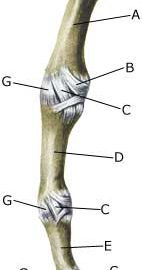
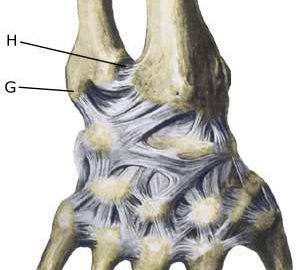
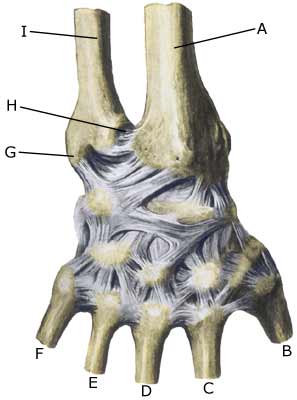
RUPTURE OF THE INNER LIGAMENT IN THE METACARPOPHALANGEAL JOINT OF THE THUMB
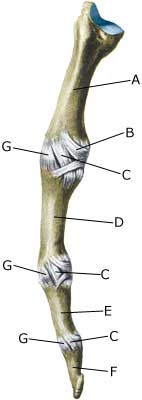
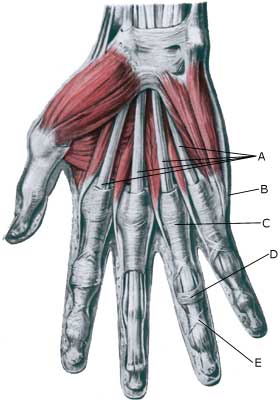
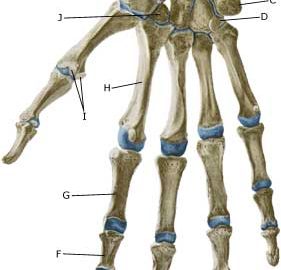
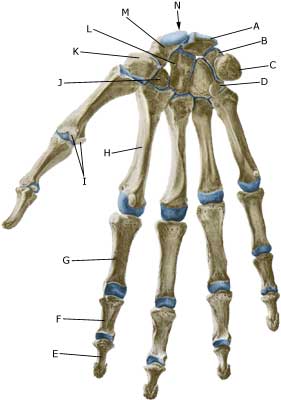
Cause: A blow, twisting or overstretching can result in a ligament rupture occurring. In some cases a piece of bone can become detached where the ligaments fasten on the side of the bone. The rupture often occurs when skiers fall and their thumb is forced back and outwards (e.g. if it is caught in the ski stick). The injury is also called “Skier’s thumb”. Symptoms: With a ruptured ligament there will often be a swelling of the joint and tenderness on the inner side. The joint feels loose and it is difficult to turn a key in the door or hold a piece of paper between the thumb and index finger. Acute treatment: Click here. Examination: It is advisable for everyone with sudden powerful pains in the thumb to have the joint examined to ensure the correct diagnosis and treatment. The results are best if the diagnosis is made and treatment is commenced immediately after the injury (article). Treatment: Most ligament ruptures internally in the thumb, with clear looseness, require surgery. It may be necessary with an X-ray examination, ultrasound (article) or an MR scan (article). Rehabilitation: Fitness training in the form of cycling and running, along with rehabilitation according to the guidelines under rehabilitation, general, can usually be commenced immediately. Once the pain is completely gone you can participate in sports activity, although handball, volleyball, basketball and similar activities should be avoided for a few additional weeks. Bandage: You will often be able to stabilize the joint with tape (tape-instruction) . Complications: In the vast majority of cases the ligaments heal without complications. In case of lasting pain and lack of progress you should consult your doctor again. |