|
Results of non-operative and operative treatment of humeral shaft fractures. A series of 104 cases. |
Kategoriarkiv: Arm. Upper
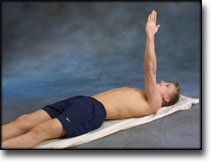
step4
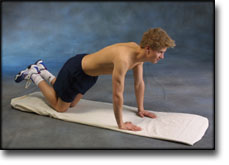
Training ladder for:
RUPTURE OF MUSCLE ON THE FRONT OF THE UPPER ARM
(RUPTURA MUSCULI BICEPS BRACHII)
STEP 4 |
Unlimited: Cycling. Swimming. Running.
|
|||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
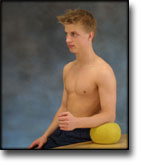
step3
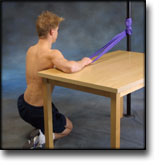
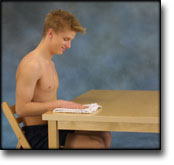
Training ladder for:
RUPTURE OF MUSCLE ON THE FRONT OF THE UPPER ARM
(RUPTURA MUSCULI BICEPS BRACHII)
STEP 3 |
Unlimited: Cycling. Swimming. Running.
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
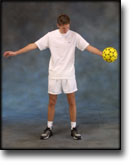
step2
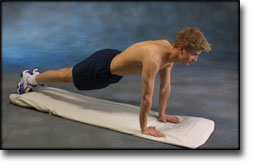
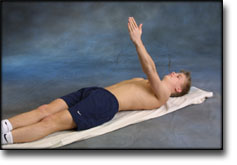
Training ladder for:
RUPTURE OF MUSCLE ON THE FRONT OF THE UPPER ARM
(RUPTURA MUSCULI BICEPS BRACHII)
STEP 2 |
Unlimited: Cycling. Running.
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
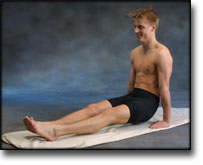
step1
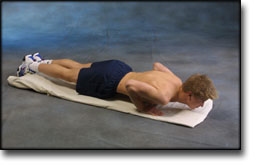
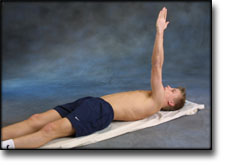
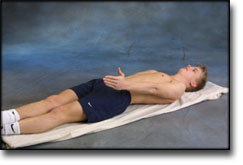
Training ladder for:
RUPTURE OF MUSCLE ON THE FRONT OF THE UPPER ARM
(RUPTURA MUSCULI BICEPS BRACHII)
STEP 1 |
| The indications of time after stretching, coordination training and strength training show the division of time for the respective type of training when training for a period of one hour. The time indications are therefore not a definition of the daily training needs, as the daily training is determined on an individual basis.
|
|||||||||||||||||||||||||||||||||||||||||||
|
Stretching is carried out in the following way: stretch the muscle group for 3-5 seconds. Relax for 3-5 seconds. The muscle group should subsequently be stretched for 20 seconds. The muscle is allowed to be tender, but must not hurt. Relax for 20 seconds, after which the procedure can be repeated. The time consumed for stretching, coordination and strength training can be altered depending on the training opportunities available and individual requirements. |
treatment-article3
|
Biceps tendon: diagnosis, therapy and results after proximal and distal rupture. |
treatment-article2
|
Management of acute and chronic biceps tendon rupture. |
treatment-article1
|
Partial rupture of the distal biceps tendon. |
examination-article2
|
Distal biceps tendon injury: MR imaging diagnosis. MATERIALS AND METHODS. RESULTS. CONCLUSION. |
examination-article1
|
Sonography of tears of the distal biceps tendon. CONCLUSION. |