|
||
|
||
 |
||
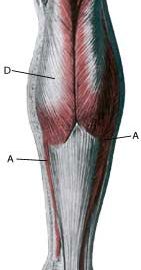
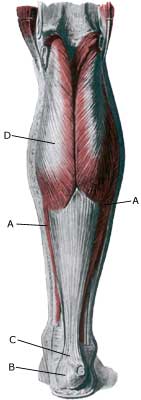
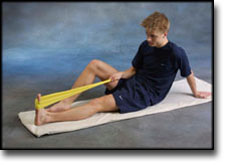
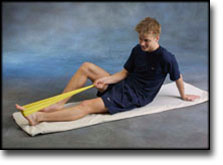
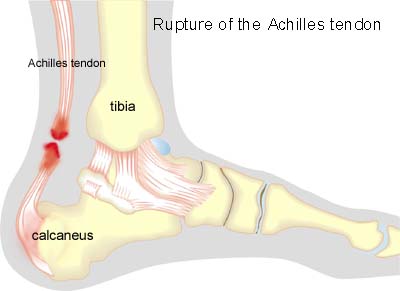
| Cause: Full or partial rupture of the Achilles tendon most usually occurs when the Achilles is stretched simultaneously with the calf muscle contracting (eccentric contraction), which happens for example when a badminton player lands after a smash and at the same time starts out to reach the net quickly. Full or partial rupture of the Achilles always occurs with the background of degeneration in the tendon. Under half the cases have experienced symptoms prior to the rupture, however, as good as all the tendons show signs of degeneration during the subsequent examination.
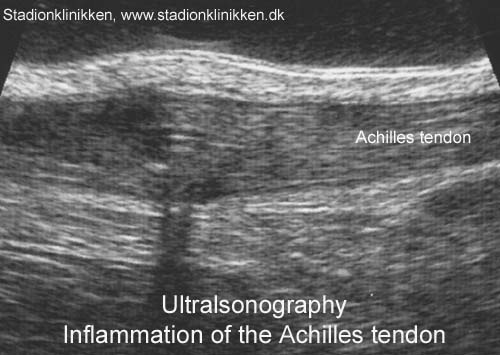
Symptoms: Sudden pain in the Achilles tendon, where there is often a sensation of feeling and hearing a “crack”. Many believe that they have been kicked from behind. The pain is aggravated when activating the Achilles (walking), pressure on the tendon and when stretching the tendon. It is often possible to feel a defect in the tendon, and it is usually impossible to walk on the toes. Acute treatment: Click here. Examination: In all cases when there is a sense of a “crack”, or sudden shooting pains in the Achilles tendon, medical attention should be sought as soon as possible. Ultrasound scanning is used to advantage when making the diagnosis, as even full ruptures can easily be overlooked without the aid of ultrasound scanning. Ultrasound scanning enables an evaluation of the extent of the change in the tendon; full or partial rupture, inflammation of the tendon (tendinitis), development of cicatricial tissue (tendinosis), clacification, inflammation of the tissue surrounding the tendon (peritendinitis) and inflammation of the bursa (bursitis) (article), (Ultrasonic image). Treatment: Ruptures can be treated with bandaging or surgical intervention. Operation is usually recommended for athletes and others with physical work. A period of 9-12 months must in all cases be expected to elapse before the sports activity can be resumed on the same level. Shoes with a slight heel elevation will relieve the pressure on the Achilles tendon. Treatment with ice for a period of at least 20 minutes after straining the tendon is recommended as long as the tendon remains sore (article-1), (article-2), (article-3). Bandage: Taping to relieve problems with the Achilles tendon is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction). Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude a renewed rupture of the Achilles tendon or: It is unfortunately often the case that it is not possible to return to the same level of sports activity despite correctly administered treatment and training. Special: As there is a risk that the injury can be permanent, all cases should be reported to your insurance company. It is important that running shoes fit well (tight heel cap, slight heel elevation, shock absorbing soles). |