|
||
|
||
|
||
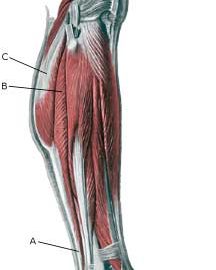
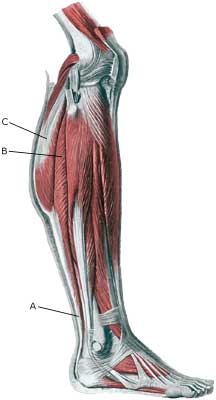
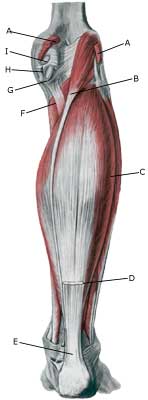
| Cause: Full or partial rupture of the soleus muscle usually occurs when the calf muscle becomes stretched while it is contracting (eccentric contraction). Partial ruptures represent the majority of the ruptures. The rupture occurs in many instances at the point of attachment of the soleus muscle to the Achilles tendon, which will often trigger an inflammation of the Achilles tendon as a result of the soleus rupture.
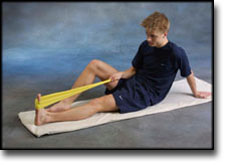
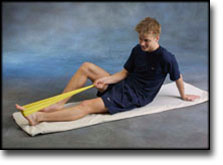
Symptoms: Pain when activating the calf muscle (running and jumping), when applying pressure on the Achilles tendon approx. 4 cm. above the anchor point on the heel bone or higher up in the calf muscle, and when stretching the tendon. Walking on tip-toe will aggravate the pain. Acute treatment: Click here. Examination: In all cases when there is a sense of a “crack”, or sudden shooting pains in the Achilles tendon, medical attention should be sought as soon as possible. Ultrasound scanning or MRI examination is used to advantage when making the diagnosis, as even full ruptures can easily be overlooked by normal clinical examination. Treatment: Treatment of the rupture can comprise rest, stretching and training. Complications: If there is not a steady improvement in the condition an ultrasound scan should be performed to exclude: |