CORTICOSTEROIDS
Injection of corticosteroid in sports-medicine is used as a result of the following indications:
- Reduction of the acute inflammation of the bursa (bursitis), inflammation of the tendon sheath (tenosynovitis) or concentration of fluid in the joint (traumatic arthritis/synovitis)
- Reduction of the damaging effect of chronic inflammation in certain protracted over-load injuries, especially inflammation of the tendon (tendinitis), and inflammation of the tissue surrounding the tendons (peritendinitis).
No other legal treatment of sports injuries has been so controversial as localised injection of corticosteroid. There is, however, no documentation that injection of corticosteroid in the area surrounding the tendons, in the joint or in the bursae should be harmful (article) (article). Although laboratory tests do indicate an immediately weakening in the tendon tissues shortly after the injection (article), human studies show no sign thereof (article). Injections direct into the tendons should be advised against however, as certain animal studies suggest that the tendon is thereby weakened (article).
Indications. Arthritis (swelling of joints due to rheumatism). Injection of corticosteroid in the joint is one of the treatments most commonly used in rheumatic illnesses. Placebo controlled studies have documented the effect of this form of treatment.
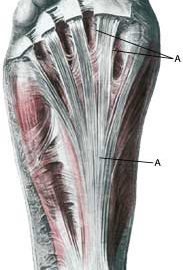
Chronic over-load symptoms from tendons. The chronic changes in the tendons are properly a mix of wear (degeneration) and inflammation (article). There are several scientific studies which documents the short term effect of corticosteroid injection around the overloaded tendons almost every where in the body. Almost all patients experienced fewer symptoms and (partial) normalisation of the chronic thickened tendons simultaneous with the disappearance of the inflamed blood vascularisation, however, a significant number experienced a relapse of the symptoms, possibly due to a much too short rehabilitation period. The way to fast rehabilitation after the injection of corticosteroids (after the pain has disappeared but before the tendon has strengthened) could also be a result as to why corticosteroids are more effective than different types of rehabilitations in the first 3 months, while rehabilitation is more effective than corticosteroids after 6 months (article). This is why it is very important that the treatment with corticosteroids are accompanied with prolonged rehabilitation (even if the discomfort fades after 1-2 months) over (more than) a half year.
Inflammation of the tissue surrounding the tendons, myositis ossificans (calcification in muscles after bleeding), bursitis and muscle rupture. Only a modest amount of documentation is available regarding treatment of these injuries with corticosteroid injection, despite the treatment being widespread.
Mechanism of action. The mechanism of action is not fully clarified.
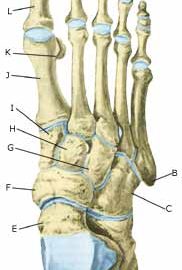
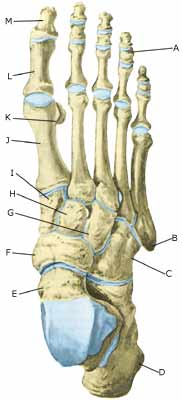
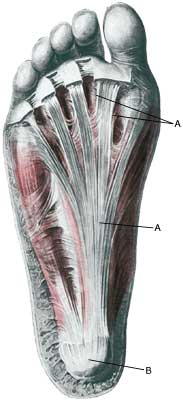
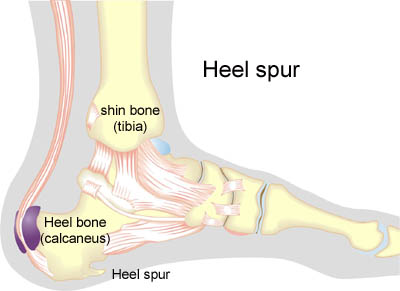
Side effects. The risk of infection is minimal with the observance of simple sterile procedures (disinfection with surgical spirits at least twice, sterile equipment, “non-touch technique”). Bleaching of the skin above the infection with visible blood vessels in the skin, a change in the sensitivity of the area, and partial loss of fatty tissue are frequent occurrences, but only in very rare cases give any discomfort. The majority of discomfort disappears spontaneously after several months (years). The risk of systematic effect following injection of corticosteroid is shown by facial blushing (about 10 %), menstruational disorder and fluctuation of blood sugar which is seen quite frequently while serious side effects like allergic shocks are extremely rare. Erroneous injection direct into the tendons as well as injection surrounding partial (and total) ruptured tendons can occour. It is for this reason that ultrasound scanning is recommended prior to all injections in areas where there are large tendons (Achilles tendon, knee cap tendon, hollow foot tendon), to ensure the correct diagnosis and exclude partial ruptures. If injections are given under the guidance of ultrasound, it will ensure the correct injection and optimal effect whilst minimising the risk. The athlete should be advised of the risk of tenderness in the area for a while after the injection (fading away during the course of a few hours or days). Local treatment with corticosteroids is allowed by the doping law.
Contraindications. Suspicions of infection in the vicinity of the place of injection and active tuberculosis. As there is only modest experience of the effects of corticosteroid injections on children, this treatment is seldom indicated for minors.
Administration. The corticosteroid is mixed with local anaesthetic prior to injection, thereby reducing the risk of side effects. The temporary subduing of pain (due to the local anaesthetic) will furthermore aid the confirmation (or the disconfirmation) of the diagnosis. Systemic treatment (tablets, suppositories, injections in the muscles and veins for systemic effect) with corticosteroid is not permitted in sport.
Discussion. Injections with corticosteroid in the area surrounding tendons can amongst other things be used as a supplement to treatment for chronic over-load conditioned tendon injuries. The basis treatment is “active rest” with increasing load within the pain threshold. If the athlete does not follow the rehabilitation principles and instead forces the rehabilitation, the chronic inflammation, the lengthy rest period and the suddenly increased training load will present a risk of rupturing the tendon.
Ultrasound scanning is recommended in treatments with injection of corticosteroid in the area surrounding larger tendons. If there is no positive effect (or the effect is passing despite correct rehabilitation) following the first ultrasound-guided injection, there are no grounds to repeat the process. If there is positive, but only partial, effect, the injection can be repeated once or twice with a minimum interval of four weeks.
Conclusion. Localised injection of corticosteroid is considered effective as treatment for bursitis, chronic inflammation of the tendon (tendinitis), inflammation of the tendon sheath (tenosynovitis), inflammation of the tissue surrounding the tendons (peritendinitis) and fluid accumulation in the joints (traumatic arthritis/synovitis), although the scientific documentation is incomplete.
On a correct indication following verification of the diagnosis with ultrasound scanning, ultrasound-guided injection of corticosteroid in the area surrounding the tendons could be an useable supplement to the basis treatment (rehabilitation) if correct rehabilitation haven’t made a progress.
The short term effect of the treatment is well documented but not for the long term effect which is only available through long term controlled rehabilitation.
If the treatment is misused to allow the athlete to continue a potentially damaging sports activity, the treatment will indirectly increase the risk of the chronic injury and tendon ruptures.
Resumé. Medicinal treatment is only a supplement to the basis treatments of sport injuries. Used the right way, the medicinal treatment can reduce the relieving period thereby starting the rehabilitation faster. If the treatment is abused to continue a harming sports activity without corrective training measurements, the risk of chronic injuries will increase.