|
||
|
||
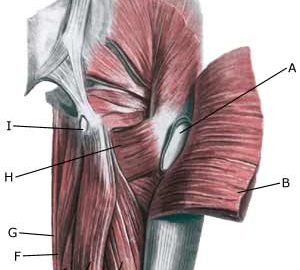
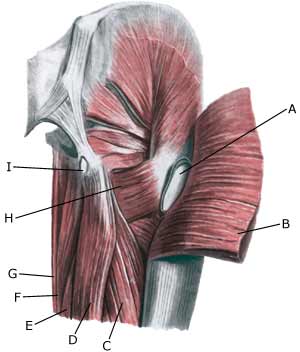
| Cause: Inflammation of the tendon fastenings (tendinitis) at the ischiatic bone (tuber ischiadicum) occurs following repeated uniform (over)loads (e.g. running, sprinting) causing microscopic ruptures in the tendon, and especially at the tendon fastening. Tendinitis is a warning that the training performed is too strenuous for the muscles in question, and if the load is not reduced a rupture of the posterior thigh muscle fastening on the ischiatic bone (“pulled muscle”) may occur. This will result in a considerably prolonged rehabilitation period.
Symptoms: Pain in the ischiatic bone can occasionally radiate down into the rear of the thigh. The pain is aggravated when applying pressure on the bone (e.g. sitting position), stretching and activating the posterior thigh muscles (flexing the knee against resistance). Acute treatment: Click here. Examination: In slight cases with only minimal tenderness and no discomfort with walking, medical examination is not necessarily required. The extent of the tenderness is, however, not always a mark of the degree of the injury. In cases of more pronounced pain or tenderness, medical examination is required to ensure the correct diagnosis and treatment. The diagnosis is usually made on the basis of a normal medical examination, however, if there is any doubt concerning the diagnosis, this can be confirmed by ultrasound scanning or MR scanning (article). Treatment: The treatment usually comprises relief, stretching and rehabilitation (article). If the rehabilitation does not progress satisfactorily, medicinal treatment in the form of rheumatic medicine (NSAID) can be considered, or corticosteroid injection in the area surrounding the inflamed tendon fastening on the ischiatic bone. As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or ruptures. The tendon can naturally not sustain maximal load after a long-term injury period and only a short-term rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected. If satisfactory progress is not made following the rehabilitation and medicinal treatment, surgical intervention can be considered. Long-term results of operations are often disappointing, despite publication of a minor series with good results (article). Complications: If the treatment does not progress according to plan, it should be considered if the diagnosis is correct or whether complications have arisen. The following should in particular be considered:
|