| Diagnosis: |
(Osteochondral lesion) |
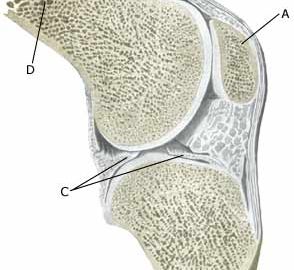
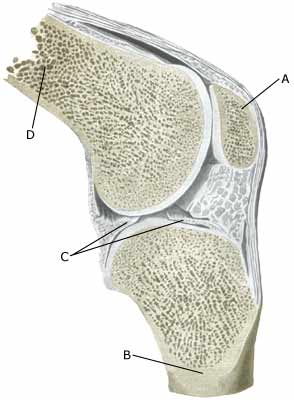
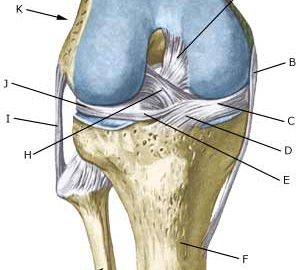
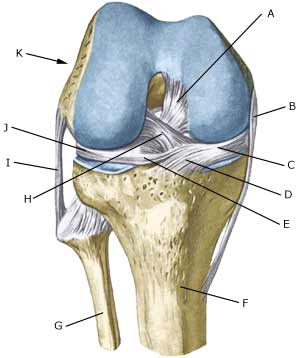
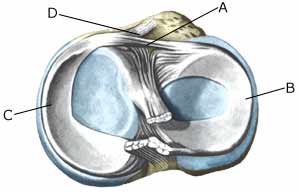
Anatomy: The bones in the knee joint comprise the thigh bone (femur), shin-bone (tibia) and the knee cap (patella). The articular surfaces of the thigh bone, shin-bone and knee cap are lined with a cartilage covering of a few millimetre’s thickness which serves to reduce the load or strain on the joint surfaces.
Cause: Twists in the knee joint causing the thigh bone and shin bone to collide can cause damage to the cartilage in the knee. In some cases a piece of cartilage can be shed which can wander in the joint (joint-mouse) and become inflamed and increase the production of synovial fluid.
Symptoms: Pain in the joint when under load or strain. Often, periodic swelling of the joint (synovitis).
Examination: Normal medical examination is often not sufficient. To make the diagnosis correctly it is therefore necessary to perform an arthroscopic examination (telescopic examination of the joint (Photo) or an MR-scanning (Ultrasonic image).
Treatment: Treatment comprises relief from the painful activities until the pain is no longer experienced, after which gradual re-training can be commenced. There is no treatment that can restore the damaged cartilage, which has itself poor restorative ability. Different procedures to enhance the healing can be attempted using arthroscopy, however, the results are generally unsatisfactory. Results from experimental cartilage transplants are still not successful enough to warrant introduction as a routine treatment in the near future (article). Joint-mouse that provokes the symptoms must be surgically removed. Injection of corticosteroid in the knee joint, performed under ultrasound guidance, can be attempted to combat prolonged and pronounced cases of fluid accumulation in the knee joint (synovitis).
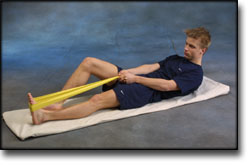
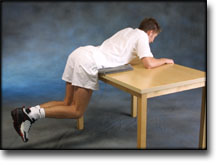
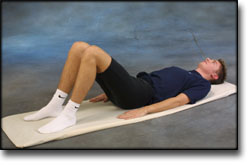
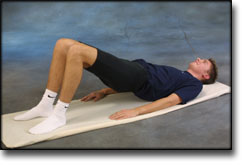
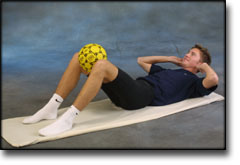
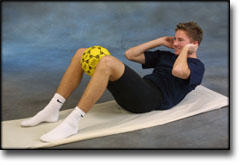
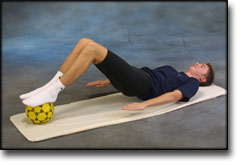
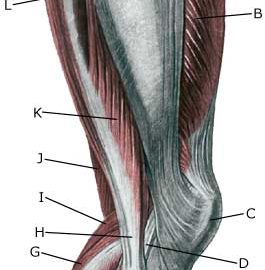
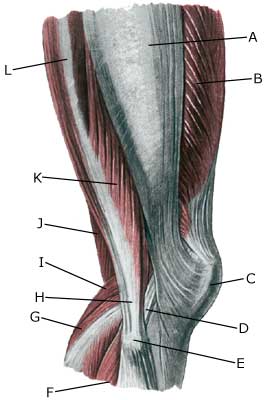
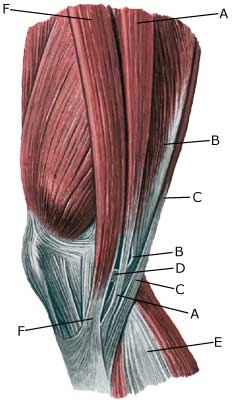
Rehabilitation: Rehabilitation is completely dependent upon the type of cartilage damage (size and position in the joint) and treatment (conservative or surgical). It is generally attempted to strengthen the musculature around the knee joint.
Also read rehabilitation, general.
Complications: Large cartilage damage which is positioned on the weight-bearing parts of the joint represents one of the most serious sports injuries, and often results in an end to the sporting career.
Special: As there is a risk that the injury can cause permanent disability, all cases should be reported to your insurance company.
|