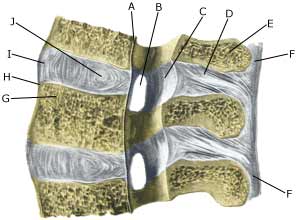
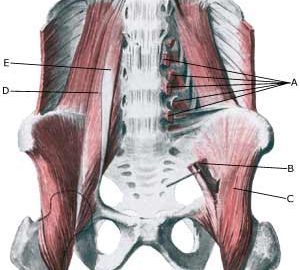
| Cause: If the back is subjected to a load which exceeds its capabilities, over-load conditioned pain will be triggered from the muscles, tendons, ligaments, and possibly from the cartilage discs (disci) and bones. Pain in the lower back is one of the most frequent sports injuries (comprises approx. 10% of injuries in a top flight football club).
Symptoms: Pain and stiffness in the lower back (lumbago), occasionally radiating to the leg (“sciatica”).
Examination: Slight back discomfort does not necessarily require medical examination, however, all cases with strong or repeated back pain should be examined. The doctor will be able to evaluate whether further examination is required, i.e. x-ray, CT or MRI scan.
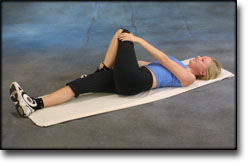
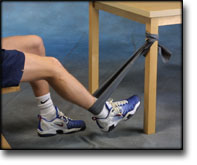
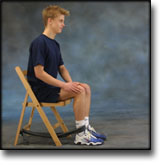
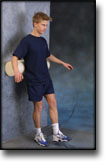
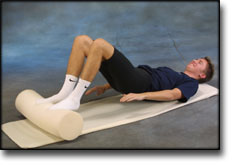
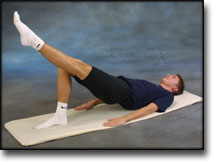
Treatment: Treatment will primarily be directed at altering the imbalance between the load the back is subjected to, opposed to the level the back is trained to manage. It is therefore recommended that you are instructed (possibly by a physiotherapist) in the appropriate way to put a strain on the back, and which loads and movements should be avoided (“ergonomic guidance”). A few days’ rest and relief may be needed to subdue the pain, after which steadily increasing training should be started with back and stomach stabilising and strengthening exercises. If painkillers are required, paracetamol can be recommended, possibly combined with rheumatic medicine (NSAID). Chronic back pain may suggest stronger painkillers, however, stronger medicine should be used with extreme caution as it can quickly lose its effect and there is a risk of increased dependence on the medicine. With acute lumbago without signs of a slipped disc, assistance can be sought from manipulative treatment by a doctor, physiotherapist or chiropractor.
Complications: If the pain does not decline under the treatment, clinical (re)examination by a doctor should be performed. Special consideration should be given to:
However, many other causes of lumbago are found, of which some will require further examination. In the majority of cases, the treatment will be identical. It will not be possible for some to be completely free of discomfort (i.e. with heavy degenerative arthritis in the lumbar region), and the aim of the treatment will often be to reduce the frequency and degree of pain.
Special: Training should be performed on a “lifelong” basis to reduce the risk of relapse after a successful rehabilitation. Smoking causes increased risk of lumbago by reducing the flow of blood to the cartilage discs (disci), implying that daily small injuries do not heal so well. Stopping smoking is therefore an important part of the treatment. Shock absorbing shoes or insoles will reduce the load on the back.
|