|
Surgical repair of chronic complete hamstring tendon rupture in the adult patient. |
Kategoriarkiv: _Tendonitis at the ischiatic bone.
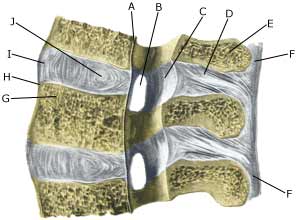
Slipped disc
|
||
|
||
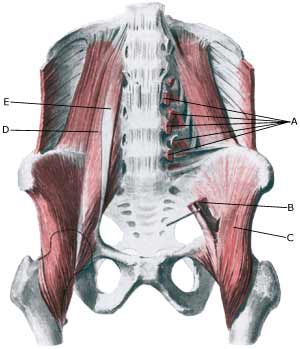
| Cause: If the back is subjected to a load which exceeds its capabilities, a crack in one of the discs may occur so that the liquid content in the centre of the disc (nucleus pulposus) can be squeezed out and apply pressure on a nerve root.
Symptoms: Pain and stiffness in the lower back (lumbago), radiating to one of the legs. There can be sensory interference and reduction in strength of the leg. Symptoms are often aggravated by coughing. In rare cases the nerves can be so severely compressed that problems can arise in control of bladder and bowels, requiring acute surgical treatment. Examination: If a slipped disc is suspected medical attention should be sought at once to establish the diagnosis and which treatment should be initiated. Treatment: If examination reveals signs of a slipped disc without alarming symptoms (problems in control of bladder and bowels or substantial deterioration of muscle/paralysis), treatment will primarily be directed at altering the imbalance between the load the back is subjected to, opposed to the level the back is trained to manage. It is therefore recommended that you are instructed (possibly by a physiotherapist) in the appropriate way to put a strain on the back, and which loads and movements should be avoided (“ergonomic guidance”). A few days’ rest and relief may be needed to subdue the pain, after which steadily increasing training should be started with back and stomach stabilising and strengthening exercises. If painkillers are required, paracetamol can be recommended, possibly combined with rheumatic medicine (NSAID). Chronic back pain may suggest stronger painkillers, however, stronger medicine should be used with extreme caution as it can quickly lose its effect and there is a risk of increased dependence on the medicine. By far the majority of slipped discs can be managed through correct training (article 1). In cases where the above treatment does not produce progress in the condition, a CT or MRI scan will be considered with a view to possible operation. CT and MRI scan and operation is therefore first considered if the rehabilitation programme does not succeed (article 2). In cases with alarming symptoms (problems in control of bladder and bowels or substantial deterioration of muscle/paralysis) acute hospitalisation is recommended for evaluation of the need for acute surgery. Special: Training should be performed on a “lifelong” basis to reduce the risk of relapse after a successful rehabilitation. Smoking causes increased risk of lumbago by reducing the flow of blood to the cartilage discs (disci), implying that daily small injuries do not heal so well. Stopping smoking is therefore an important part of the treatment. Shock absorbing shoes or insoles will reduce the load on the back. |

Lumbago
|
||
|
||
| Cause: If the back is subjected to a load which exceeds its capabilities, over-load conditioned pain will be triggered from the muscles, tendons, ligaments, and possibly from the cartilage discs (disci) and bones. Pain in the lower back is one of the most frequent sports injuries (comprises approx. 10% of injuries in a top flight football club).
Symptoms: Pain and stiffness in the lower back (lumbago), occasionally radiating to the leg (“sciatica”). Examination: Slight back discomfort does not necessarily require medical examination, however, all cases with strong or repeated back pain should be examined. The doctor will be able to evaluate whether further examination is required, i.e. x-ray, CT or MRI scan. Treatment: Treatment will primarily be directed at altering the imbalance between the load the back is subjected to, opposed to the level the back is trained to manage. It is therefore recommended that you are instructed (possibly by a physiotherapist) in the appropriate way to put a strain on the back, and which loads and movements should be avoided (“ergonomic guidance”). A few days’ rest and relief may be needed to subdue the pain, after which steadily increasing training should be started with back and stomach stabilising and strengthening exercises. If painkillers are required, paracetamol can be recommended, possibly combined with rheumatic medicine (NSAID). Chronic back pain may suggest stronger painkillers, however, stronger medicine should be used with extreme caution as it can quickly lose its effect and there is a risk of increased dependence on the medicine. With acute lumbago without signs of a slipped disc, assistance can be sought from manipulative treatment by a doctor, physiotherapist or chiropractor. Complications: If the pain does not decline under the treatment, clinical (re)examination by a doctor should be performed. Special consideration should be given to:
However, many other causes of lumbago are found, of which some will require further examination. In the majority of cases, the treatment will be identical. It will not be possible for some to be completely free of discomfort (i.e. with heavy degenerative arthritis in the lumbar region), and the aim of the treatment will often be to reduce the frequency and degree of pain. Special: Training should be performed on a “lifelong” basis to reduce the risk of relapse after a successful rehabilitation. Smoking causes increased risk of lumbago by reducing the flow of blood to the cartilage discs (disci), implying that daily small injuries do not heal so well. Stopping smoking is therefore an important part of the treatment. Shock absorbing shoes or insoles will reduce the load on the back. |
Fluid accumulation in the hip joint
Cause: Many repeated loads or one violent load can cause an inflammation of the synovial membrane (synovitis), fluid formation, swelling, restriction of movement and pain in the hip joint. The condition is relatively often seen in children (Ultrasonic image). Symptoms: Pain in the joint upon movement with load. Often there will be movement restriction with rotation of the hip joint. Examination: It will often be necessary to supplement the ordinary clinical examination with an ultrasound scan, where the fluid in the hip joint can easily be seen (Ultrasonic image). Treatment: The treatment primarily comprises relief from the pain inducing activity until the swelling has abated. Rehabilitation, within the pain threshold, can subsequently be commenced. In cases of lack of progress with relief the treatment can be supplemented with a medical treatment in the form of rheumatic medicine (NSAID) or by drainage of the joint fluid and the injection of corticosteroid, which should be done with ultrasound guidance. Complications: In particular you should consider a bacterial infection in the joint (pyarthron), which is determined by ultrasound guided draining of the joint fluid, the child hip diseases (epifysiolysis capitis femoris and Calvé-Legg-Perthes disease), where the joint head on the femur slips or collapses (X-ray examination will determine the diagnosis), arthritis or:
Special: There are two childrens’ hip diseases that should always be considered in children with hip pain.
|
Inner snapping hip
|
||
|
||
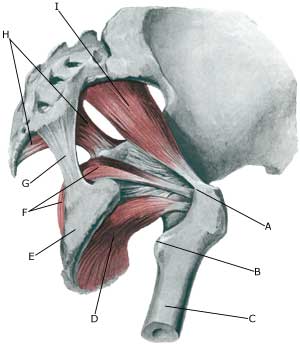
| Cause: In case of repeated loads the muscle tendon can become inflamed, swell and with some movements slip over the one of the bone projections at the pelvis or the hip joint. When the tendon slips over the bone projection, the uncomfortable symptoms are produced. There are three known causes of snapping hips: outer snapping hip (tractus iliotibialis), inner snapping hip (iliopsoas tendon) and joint conditioned (intraarticular) causes (article). The treatment is dependant on the cause.
Symptoms: With certain movements in the hip joint the deep hip flexor (M iliopsoas) can be made to slip over one of the bone projections on the pelvis or the hip joint, whereby a slipping sensation, often accompanied by discomfort, is felt and often heard. Acute treatment: Click here. Examination: In light cases with only minimal tenderness medical examination is not necessarily required. In case of more pronounced pain or lack of progress a medical examination should be carried out to ensure the diagnosis. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis a dynamic ultrasound scan can be performed, where the tendon can be seen slipping as this triggers the symptoms (article 1) (article 2), (article 3). Treatment: The treatment primarily comprises relief. If progress is not smooth the treatment can be supplemented with rheumatic medicine (NSAID) or the injection of corticosteroid, which should be done with ultrasound guidance to ensure the optimal effect and minimal risk. Only in very rare cases is surgical treatment necessary. Complications: If progress is not smooth it should be considered whether the diagnosis is correct or if complications have arisen. In particular the following should be considered:
|
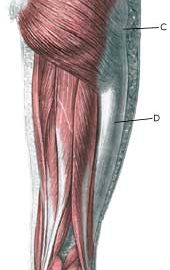
Outer snapping hip
|
||
|
||
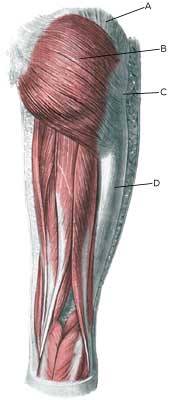
| Cause: With repeated movements in the knee and hip joint (running, dancing, gymnastics) the powerful tendon (tractus iliotibialis) slips over the outer bone projection (trochanter major) of the femur, which can cause inflammation in the tendon or in the underlying bursa. When the inflamed tendon slips over the bone projection, a sudden, slipping, and unpleasant sensation can be felt. There are three known causes of snapping hips: outer snapping hip (tractus iliotibialis), inner snapping hip (iliopsoas tendon) and joint conditioned (intraarticular) causes, Coxa Saltans: The Snapping Hip Revisited (article).
Symptoms: Upon certain movements in the hip joint, a sudden slipping, and unpleasant sensation can suddenly be produced on the outside of the thigh, which is often audible. Acute treatment: Click here. Examination: Usually the diagnosis can be made by an ordinary medical examination. You can often prevent the tendon from slipping over the outer bone projection by holding the tendon aside, while the movements provoking the condition are performed. The pain will decrease for approx. one hour after the injection of a local anaesthetic (diagnostic blockade) around the outer hip bone projection. If the diagnosis does not appear to be certain, ultrasound is recommended (Ultrasonic image), (article), or possibly a MRI scan. Treatment: The treatment primarily comprises relief, stretching of the external tendon and rehabilitation. It is crucial that shoes have good shock absorbing soles. In cases of inappropriate foot stance, this should be corrected with shoes or inlays. In case of lack of progress the treatment can be supplemented with medical treatment in the form of rheumatic medicine (NSAID) or the injection of corticosteroid, which advantageously can be guided by ultrasound. In severe cases with no effect from relief, correct rehabilitation or medical treatment, you can operatively split the tendon. Complications: In case of lack of progress it should be considered whether the diagnosis is correct. This will often require supplemental examinations (X-ray, ultrasound or MRI scan). In particular the following should be considered:
Special: Shock absorbing shoes or inlays will reduce the load. In case of lack of progress or recurrences after successful rehabilitation it can be considered to have a running style analysis performed, to evaluate whether correction of the running style is indicated. |
Degenerative arthritis in the hip joint
Cause: In case of repeated loads, the cartilage primarily, and subsequently the bone below the cartilage, can be damaged (degenerative arthritis). The degenerative arthritis changes can in some cases cause an inflammation of the synovial membrane (synovitis) which causes fluid formation, swelling, movement restriction and pain in the hip joint. Symptoms: Pain in the hip joint upon movement with load. There will often be movement restriction upon rotation in the hip joint. Examination: Ordinary clinical examination is often sufficient to make the diagnosis. The examination can be supplemented with an X-ray examination. Ultrasound scan is the most suitable examination if you suspect a fluid accumulation in the hip joint. Treatment: The treatment primarily comprises relief from the pain inducing activity until any swelling in the hip joint has decreased. Rehabilitation can subsequently be commenced with the primary goal to strengthen the muscles around the hip joint and preserve the joint mobility. There is no treatment that can restore the ruined cartilage (and bone). Cartilage transplants are not yet suitable for general degenerative arthritis changes. Upon swelling in the hip joint you can attempt to reduce the synovitis with rheumatic medicine (NSAID) or by attempting to drain the fluid and injecting corticosteroid, which should be conducted with ultrasound guidance to optimise the effect and minimize the risk. Pain without joint swelling is best treated with paracetamol. In cases of severe degenerative arthritis changes with pain when resting (at night) it may be necessary to replace the hip joint. Complications: Degenerative arthritis which sits on the weight bearing parts of the joint is one of the most serious sports injuries, and often results in a termination of active sport. Cycling and swimming are significantly less stressful for the hip joint than running. In particular the following should be considered:
Special: Shock absorbing shoes or inlays will reduce the load. |
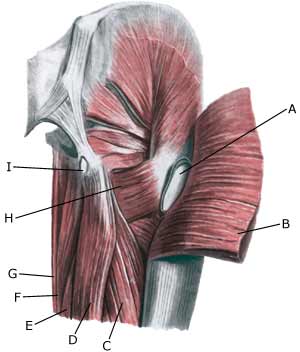
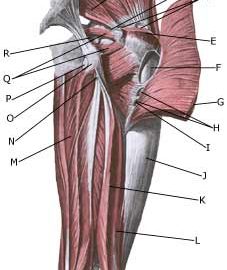
Piriformis syndrom
|
||
|
||
| Cause: If the muscle is over-loaded, it will become taut and tender. In some cases, the muscle can become so taut that it jams against the ischias nerve (nervus ischiadicus).
Symptoms: Pain deep in the buttock, with periodic radiation into the leg. Examination: The diagnosis will be rendered probable under clinical examinations by demonstrating tenderness by applying pressure on the muscle deep within the buttock, as well as provoking pain by stretching and activating the muscle. There is no suitable method to provide a pictorial image of the muscle (MR scanning can be attempted in the event of suspicions of nerve impingement) (article). Treatment: The treatment usually comprises stretching and subsequent strength training of the muscles surrounding the lower back and buttocks. It is only in very rare cases involving nerve impingement that surgery is indicated. Uncomfortable pain can be treated medicinally in the form of paracetamol, or possibly rheumatic medicine (NSAID) . If this treatment does not provide the desired relief, ultrasound guided injection of corticosteroid in the most tender part of the muscle can be attempted (article 1), (article 2). Special: Shock absorbing shoes or inner inlays will reduce the risk of various forms of muscle infiltrations. In the event of unsatisfactory progress, or relapse after successful rehabilitation, consideration must be given to performing an analysis of the patient’s running style to establish whether a correction of the running style should be recommended. Complications: If progress is not smooth, the correctness of the diagnosis should be considered or whether complications have arisen. The following should be considered in particular:
|
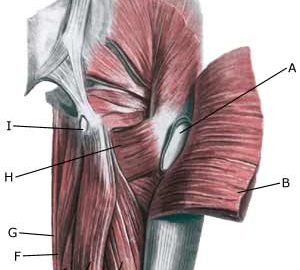
Bursitis at the outer femoral bone projection (bursitis trochanterica)
|
||
|
||
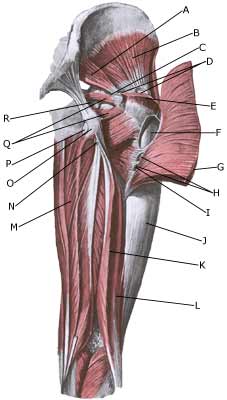
| Cause: In case of repeated loads or blows the bursa can become inflamed, produce fluid, swell and become painful.
Symptoms: Pain when applying pressure on the thigh corresponding to the bursa, which sometimes (but far from always) can feel swollen. The pain can radiate down the thigh. Acute treatment: Click here. Examination: In light cases with only minimal tenderness medical examination is not necessarily required. In case of more pronounced pain or lack of progress, a medical examination should be carried out to ensure the diagnosis and commencement of any treatment. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis an ultrasound scan can be performed (Ultrasonic image). Treatment: The treatment primarily comprises relief. If the direct cause of the complaint is known, it should of course be removed. The treatment can be supplemented with rheumatic medicine (NSAID) or injection of corticosteroid in the bursa, which is best performed under the guidance of ultrasound. Complications: If progress is not smooth, the correctness of the diagnosis should be considered or whether complications have arisen:
Special: Shock absorbing shoes or inlays will reduce the load. In case of lack of progress or recurrences after successful rehabilitation it can be considered to have a running style analysis, to evaluate whether correction of the running style is indicated. |
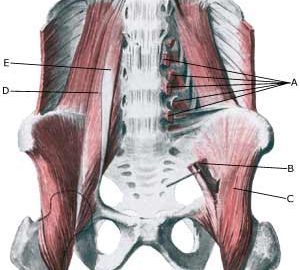
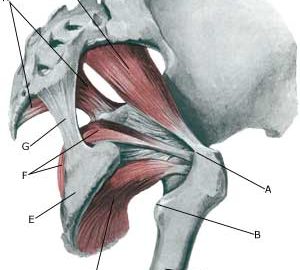
Muscle rupture of the tendon fastening on the ischiatic bone
|
||
|
||
| Cause: When a muscle is subjected to a load beyond the strength of the muscle (typically sprinting), a rupture occurs. The vast majority of ruptures are partial muscle ruptures. Many of the ruptures at the muscle fastening on the ischiatic bone (tuber ischiadicum) er preceded by lengthy tendinitis (entesopatia tuber ischiadicum) at the same location. In rare cases, the muscle fastening can tear a piece of the ischiatic bone off (especially seen in children as the growth zone on the ischiatic bone (apophysis) increases the risk of tears).
Symptoms: In slight cases a local tenderness is felt after being subjected to load (“sprained muscle”, “imminent pulled muscle”). In severe cases sudden shooting pains are felt in the muscle (“partial muscle rupture”, “pulled muscle”) and in the worst case a sudden snap is felt rendering the muscle unusable (“total muscle rupture”). The following three symptoms are characteristic in connection with muscle injuries: pain upon applying pressure, stretching and activation of the muscle (flexing knee) against resistance. With total ruptures a defect and a swelling (the contracted muscle belly and bleeding) can often be seen and felt in the posterior thigh muscle just below the ischiatic bone and below. Acute treatment: Click here. Examination: In very slight cases with only minimal tenderness and no discomfort when walking, medical examination is not necessarily required. The severity of the tenderness is however, not always a measure of the extent of the injury. In cases of more pronounced tenderness or pain, medical examination is required to ensure the diagnosis and treatment. The diagnosis is usually made following normal medical examination, however, if there is any doubt concerning the diagnosis, ultrasound scanning (or MRI scanning) can be performed, as these are the most suitable examinations to ensure the diagnosis (article). The larger the bleeding as assessed by ultrasound scanning, the longer the period needed to heal the injury. Tears on the ischiatic bone will usually be visible on x-rays. Treatment: Treatment comprises relief and rehabilitation. The aim of the rehabilitation is to strengthen the posterior thigh muscles to enable the muscles to manage the loads which previously caused the rupture. It is only in very rare cases where there is a total rupture at the muscle fastening or tearing of a large piece of bone from the ischiatic bone that surgery is considered (article). Even large ruptures in the thigh muscles will usually be able to be healed and rehabilitated without giving functional disorder (but often cosmetic disfigurement with an irregular thigh muscle). Complications: If steady progress is not experienced it should be considered if the diagnosis is correct or whether complications have arisen. The following should in particular be considered:
|