




|
Risk factors for stress fractures. |
|
Less common stress fractures in the foot. |
|
||
|
||
| Cause: Degenerative arthritis occurs with repeated (over) load when first the cartilage takes damage, and then the bone under the cartilage. Degenerative arthritis can in some instances cause an irritation of the synovial membrane which will result in concentration of fluid, swelling, reduction in mobility and pain in the joints. Degenerative arthritis in the ankle joint is often seen after repeated ligament injuries (outer ankle joint ligaments, inner ankle joint ligaments), where cartilage lesions in the ankle joint have occurred at the same time.
Symptoms: Pain in the joint with movement under load. Occasionally swelling in the joint. Examination: Normal clinical examination is often sufficient. However, it is also often necessary to perform an x-ray (or ultrasound scan or MRI examination) to make the diagnosis. Ultrasound scanning will often reveal inflammation surrounding new bone development at the joint surfaces. Treatment: Treatment comprises relief from the painful activities until the swelling has gone down, after which training can commence with the primary aim to strengthen the muscles surrounding the joint and retain joint mobility. There is no treatment which can restore the damaged cartilage (and bone). Cartilage transplants are, as yet, not suitable for general degenerative arthritis. In cases of swelling in the joint, and with inflamed new bone development at the joint surfaces, inflammation of the synovial membrane can be attempted subdued by using rheumatic medicine (NSAID), or by draining the fluid and injecting corticosteroid. The injections can be performed to advantage by utilising an ultrasound guided method. Pain without swelling of the joints is best treated with paracetamol. In severe cases of degenerative arthritis where there is pain when resting (at night), it may be necessary to fix the joint by operation. Rehabilitation: Rehabilitation is completely dependent upon the degree of the degenerative arthritis and in which joints it is located. Bandage: A supportive tape (Hollywood bandage) can be attempted to aid degenerative arthritis in small joints (toes) (tape-instruction). Tape provides no help to attacks in the ankle joint. Complications: Degenerative arthritis which sits on the weight bearing parts of the joint is one of the most serious sports injuries, and often results in a termination of active sport. It is usually possible to continue sport activities with light strain on the joints (cycling, swimming), whereas it is advisable to participate in activities with great strains on the joint (running, ball games) with restraint. The diagnostic considerations in connection with degenerative arthritis include:
Special: Shoes with shock absorbing inlays will reduce the discomfort of degenerative arthritis. |
|
||
|
||
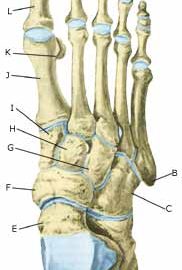
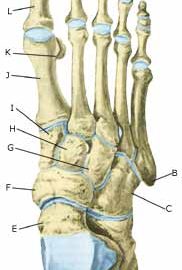
| Cause: Repeated load or strain (walking or running) can in some cases entail the load exceeding the strength of the bone tissue, thus resulting in a stress (or fatigue) fracture. Stress fractures are most often seen in the metatarsal bones, (article) (article).
Symptoms: Pain when applying pressure (direct or indirect tenderness), and when applying load or strain. Examination: X-ray examination will usually, but not always, reveal a stress fracture. The x-ray examination can be repeated after a few weeks as a number of stress fracture are not easily discernible in the early stages. Bone scintigraphy, ultrasound scanning and MRI examination can often diagnose a stress fracture much earlier than x-ray examination (Ultrasonic image), (Scintigraphy-image). Treatment: Treatment is primarily relief and rest, and possible bandaging. Surgical intervention is only required in very special cases. It is imperative that shoes are equipped with impact absorbing soles (article). Complications: If there is not a steady improvement in the condition a medical examination should be performed once more to ensure that the fracture is healing according to plan. In some cases, a false joint can develop which will require surgical treatment. |
|
||
|
||
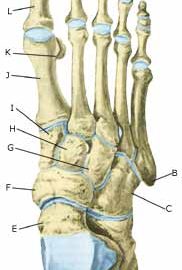
| Cause: A blow or violent twist can cause a fracture of the bone (X-ray picture).
Symptoms: Pain when applying pressure (direct or indirect tenderness), and when applying load or strain. Acute treatment: Click here. Examination: X-ray examination will usually reveal the fracture. The fracture can in some cases first be seen after 14 days, thus the x-ray examination should be repeated if there is a continued suspicion of a fracture. Treatment: Treatment is completely dependent upon which bones are broken, and whether there is a dislocation of the fracture. In some cases relief and rest without bandaging can be opted for, whereas other types of fracture require bandaging and possibly surgical intervention (article) (X-ray picture). Rehabilitation: Rehabilitation is totally dependent upon the type of fracture, and the treatment (conservative or surgical). Complications: If there is not a steady improvement in the condition a medical examination should be performed once more to ensure that the fracture is healing according to plan. In some cases, a false joint can develop which will require (renewed) surgical treatment (X-ray picture). Special: As there is a risk that the injury can cause permanent disability, all cases should be reported to your insurance company. |
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR CROOKED BACK
(SCOLIOSIS)
STEP 4 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR CROOKED BACK
(SCOLIOSIS)
STEP 3 |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||
|
||
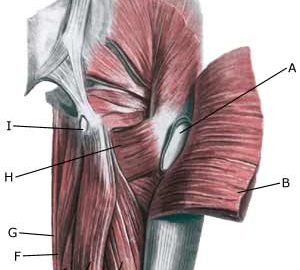
| Cause: Inflammation of the tendon fastenings (tendinitis) at the ischiatic bone (tuber ischiadicum) occurs following repeated uniform (over)loads (e.g. running, sprinting) causing microscopic ruptures in the tendon, and especially at the tendon fastening. Tendinitis is a warning that the training performed is too strenuous for the muscles in question, and if the load is not reduced a rupture of the posterior thigh muscle fastening on the ischiatic bone (“pulled muscle”) may occur. This will result in a considerably prolonged rehabilitation period.
Symptoms: Pain in the ischiatic bone can occasionally radiate down into the rear of the thigh. The pain is aggravated when applying pressure on the bone (e.g. sitting position), stretching and activating the posterior thigh muscles (flexing the knee against resistance). Acute treatment: Click here. Examination: In slight cases with only minimal tenderness and no discomfort with walking, medical examination is not necessarily required. The extent of the tenderness is, however, not always a mark of the degree of the injury. In cases of more pronounced pain or tenderness, medical examination is required to ensure the correct diagnosis and treatment. The diagnosis is usually made on the basis of a normal medical examination, however, if there is any doubt concerning the diagnosis, this can be confirmed by ultrasound scanning or MR scanning (article). Treatment: The treatment usually comprises relief, stretching and rehabilitation (article). If the rehabilitation does not progress satisfactorily, medicinal treatment in the form of rheumatic medicine (NSAID) can be considered, or corticosteroid injection in the area surrounding the inflamed tendon fastening on the ischiatic bone. As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or ruptures. The tendon can naturally not sustain maximal load after a long-term injury period and only a short-term rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected. If satisfactory progress is not made following the rehabilitation and medicinal treatment, surgical intervention can be considered. Long-term results of operations are often disappointing, despite publication of a minor series with good results (article). Complications: If the treatment does not progress according to plan, it should be considered if the diagnosis is correct or whether complications have arisen. The following should in particular be considered:
|
TRAINING LADDER FOR CHILDREN AND ADOLESCENTS:
FOR CROOKED BACK
(SCOLIOSIS)
STEP 2 |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||