JUMPERS KNEE
|
||
|
||
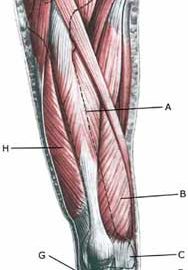
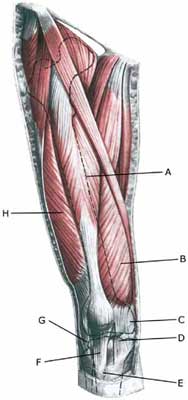
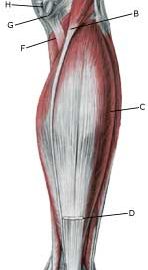
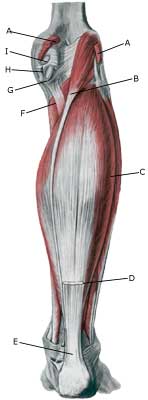
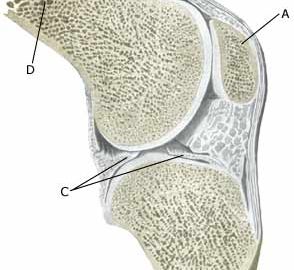
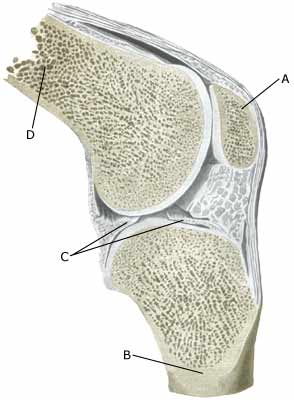
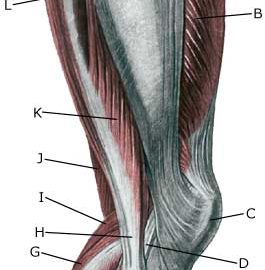
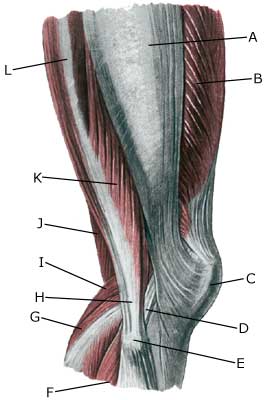
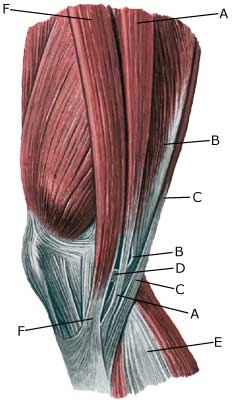
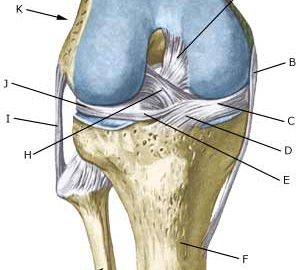
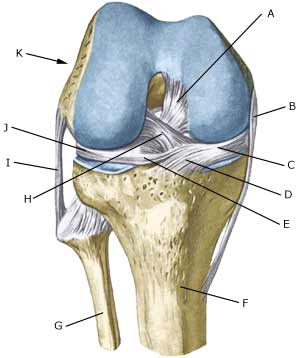
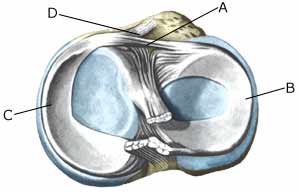
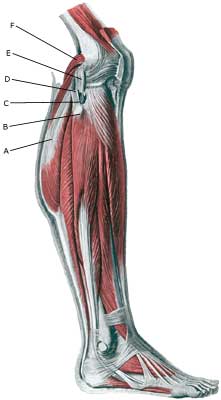
| Cause: Repeated uniform loads on the knee cap ligament (jumping, kicking) causes microscopic ruptures at the knee cap ligament fastening on the lower edge of the knee cap. As the load often continues despite tenderness, which in the early stages diminishes after warm-up, a chronic inflammation gradually occurs in the ligament. In some cases, the symptoms will arise at the ligament fastening from the anterior thigh muscle on the upper edge of the knee cap (Photo)
Symptoms: Jumping and similar activity will initially cause tenderness at the lower edge of the knee cap. The pain diminishes during the first weeks/months after warm-up. If the sport activity continues the pain will increase, resulting in the activity eventually becoming impossible. Acute treatment: Click here. Examination: Correct treatment from the outset is essential for a good result. A medical examination is consequently recommended as soon as possible after the initial onset of pain under the knee cap. The diagnosis is often made following a normal medical examination. At deterioration or lack of progress, an ultrasound scan should be performed which will be able to reveal a thickening of the ligament, granuloma, scar tissue formation, partial rupture, calcification in the ligament, bursitis and inflammation of the tissue surrounding the ligament (peridenitis) (Ultrasonic image) (article). Treatment: The treatment consists of relief from the pain inducing activity (jumping, kicking) as soon as possible after the onset of symptoms. The injury can in some cases heal within a few weeks if the treatment is instigated quickly. A rehabilitation period of several months must be anticipated if the pain has been in evidence for some months, and especially if an ultrasound scan has found thickening or changes of the ligament. Emphasis is put on stretching and strength training of the anterior thigh muscle, by activating the muscle simultaneously with stretching (eccentric training). Ice treatment can be repeated every time tenderness is provoked in the knee cap during the rehabilitation period. If there is a lack of progress following relief and strict rehabilitation, medicinal treatment in the form of rheumatic medicine (NSAID) can be considered, or injection of corticosteroid in the area surrounding the thickened part of the ligament. Research has shown that ultrasound guided injection of corticosteroid is extremely effective in reducing the extent of the thickened ligament, allowing more active rehabilitation to begin (Ultrasonic image) (article-1), (article-2). As the injection of corticosteroid is always an element in the long term rehabilitation of a very serious, chronic injury, it is vital that the rehabilitation period lasts over several months in order to reduce the risk of a relapse or rupture. The ligament is naturally unable to accommodate maximum strain or load after a prolonged injury period following only a short rehabilitation period. If the diagnosis is made by use of ultrasound scanning, the injections are performed under guidance of ultrasound, and the rehabilitation is progressed in accordance with the guidelines mentioned, then the treatment involving corticosteroid injections has very few risks connected (article). It is not unusual for a rehabilitation period of six months before maximum strain or load in the form of jumping is permitted. During recent years, different types of experimental treatment have been seen such as sclerosis injection (where injections are performed around the tendon with a drug to destroy the small blood vessels (and nerves) that infiltrate the sick tendons), and shock-wave (ultrasound treatment). However, there is no sure or clear documentation for the effect of these kinds of treatment. If satisfactory progress is not made in the rehabilitation and conservative treatment, surgical intervention can be considered. Long-term results of operations are often disappointing (article). Bandage: Some patients have the opinion that the application of tape or bandage around the shin bone directly under the knee cap can relieve the discomfort (tape-instruction). Complications: In case of lack of progress it should be considered whether the diagnosis is correct or whether complications have arisen. Special consideration should be given to:
Special: Shock absorbing shoes or inlays will reduce the load. |