MUSCLE RUPTURES AROUND THE KNEE
|
||
|
||
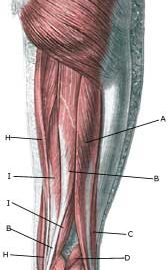
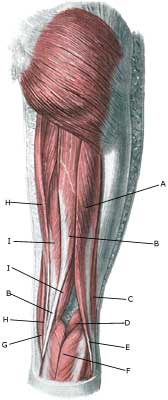
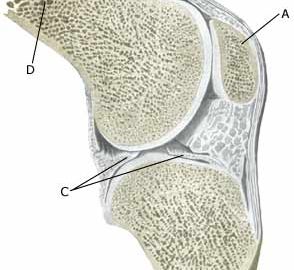
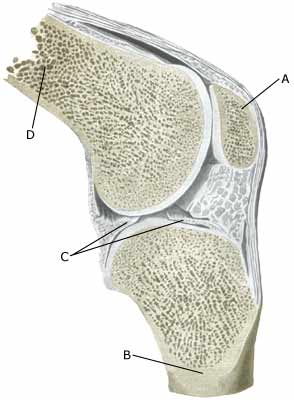
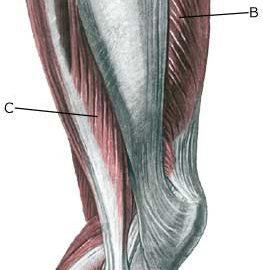
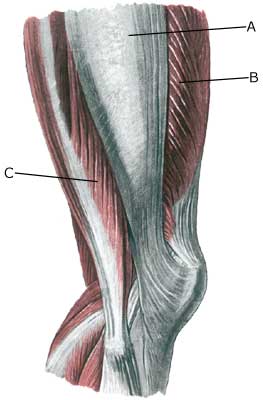
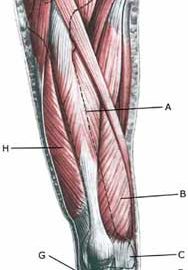
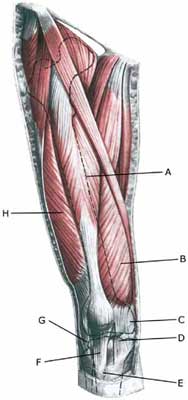
| Cause: Muscle ruptures occur following sudden, violent loads, causing a total or partial rupture in the muscle or the muscle fastening. Many muscle ruptures are preceded by tenderness in the muscle or muscle tendon. Ruptures in the anterior thigh muscle fastening (tendo m bicipitis femoris) on the head of the calf bone (caput fibulae), and the calf muscle fastenings in the popliteal space are commonly seen. The vast majority of ruptures are partial ruptures.
Symptoms: Pain when applying pressure along the muscle tendon, aggravated by stretching and activation against resistance (flexing of knee). In light cases, a local tenderness can be felt after subjecting to load (“sprained muscle” “imminent pulled muscle”). In more severe cases, a sudden shooting pain can be felt in the muscle (“partial muscle rupture”, “pulled muscle”) and in the worst cases a violent “snap” can be felt, after which it is impossible to use the muscle (“total muscle rupture”). The following three symptoms are characteristic of muscle injuries: pain when applying pressure, stretching and activation against resistance (flexing of knee). A defect in the muscle can often be seen and felt in cases of a total muscle rupture, as well as swelling in the muscle (the contracted muscle belly and muscular bleeding). Acute treatment: Click here. Examination: A medical examination is not necessarily required in light cases. More severe cases, or cases where the treatment has not brought any improvement should be evaluated by a doctor to make a precise diagnosis. The diagnosis is usually made on the basis of a normal medical examination. Ultrasound scanning (and MR scanning) is often necessary in cases of a severe rupture in order to evaluate the extent of the rupture and bleeding (Ultrasonic image). Treatment: Treatment comprises rest and relief, stretching and increasing loads within the pain threshold. Muscle ruptures are usually treated with a rehabilitation program, and surgery can only be considered in very rare cases with total muscle ruptures. Complications: In case of lack of progress it should be considered whether the diagnosis is correct. Special consideration should be given to:
|