|
||
|
||
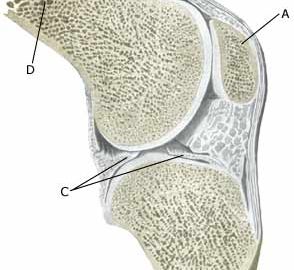
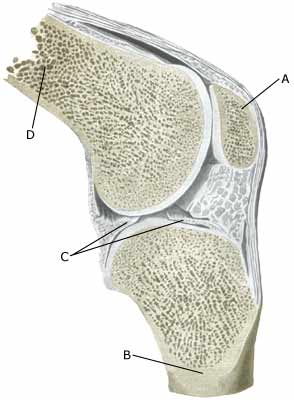
| Cause: Repeated and uniform loads can cause damage to the cartilage, and subsequently the bone beneath the cartilage (degenerative arthritis). Degenerative arthritis changes (osteoarthrosis) on the rear of the kneecap occur often after a fall on the knee and with many smaller over-loads, however, in many cases the cause is unknown. A weak thigh muscle and increased outward turning of the foot (pronation) have been suspected of being a contributory factor to the disease. The frequency of chondromallacia is dwindling, most probably due to the fact that physicians have become better at making other diagnoses (article).
Symptoms: Pain in the joint when under load or strain, especially with bent knee (for example stairway steps). A sensation of stiffness in the knee after a prolonged period of sitting. Swelling of the joint (synovitis) in occasional cases. Examination: Normal medical examination is often sufficient. A characteristic of the condition is that the pain occurs when the knee cap presses against the thigh bone, producing a rough, grating sensation. If there are any doubts regarding the diagnosis the examination can be supplemented by X-rays, arthroscopic examination or an MR-scan. (article). Treatment: Treatment comprises relief from the painful activities until the pain is no longer experienced, after which gradual re-training can be commenced primarily aimed at strengthening the thigh muscles. There is no treatment that can restore the damaged cartilage on the knee cap. For children, treatment of chondromalacia (a softening of the articular cartilage) is non-operative, as the condition has a good prognosis in the younger age groups (article). Several different surgical treatments have been attempted with unsatisfactory results (article). Bandage: Some patients have felt that the discomfort from cartilage damage behind the knee cap has been helped by applying a knee bandage that holds the knee cap slightly to the side. Alternatively, knee cap stabilising tape can be used, (tape-description). Complications: If smooth progress is not achieved it should be considered whether the diagnosis is correct, which will often require supplementary examination (X-ray, ultrasound scanning, MR scanning or arthroscopy). The following should especially be considered:
|