|
||
|
||
|
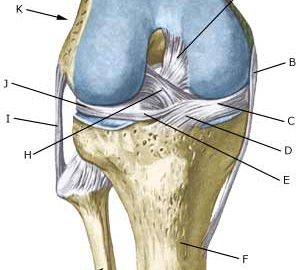
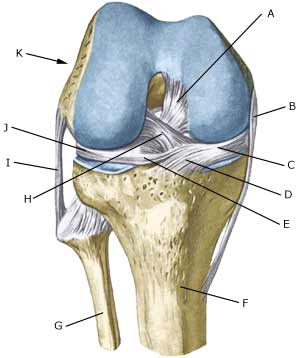
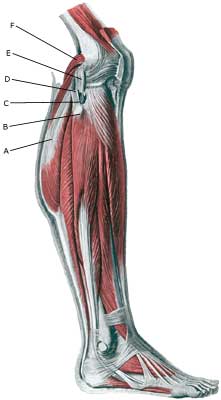
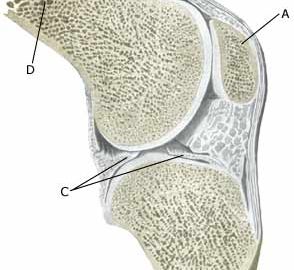
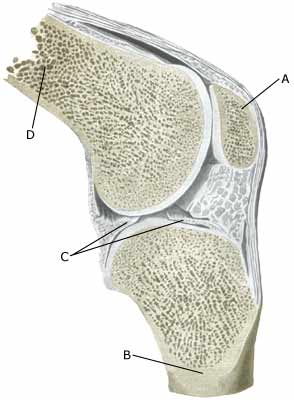
Cause: Repeated uniform loads on the knee cap ligament (jumping, kicking) causes microscopic ruptures at the knee cap ligament fastening on the lower edge of the knee cap. As the load often continues despite tenderness, which in the early stages diminishes after warm-up, a chronic inflammation gradually occurs in the ligament. In some cases, the symptoms will arise at the ligament fastening on the lower edge of the knee cap (Photo)
Symptoms: Jumping and similar activity will initially cause tenderness at the lower edge of the knee cap. The pain diminishes during the first weeks/months after warm-up. If the sport activity continues the pain will increase, resulting in the activity eventually becoming impossible. Acute treatment: Click here. Examination: The diagnosis is often made following a normal medical examination, however, if there is any doubt surrounding the diagnosis an ultrasound scan should be performed which will be able to reveal a fraying out (fragmentation) of the bone at the apex of the knee cap (aseptic necrosis of the bone) (article). Treatment: The treatment consists of relief from the pain inducing activity (jumping, kicking) as soon as possible after the onset of symptoms. The injury can in some cases heal within a few weeks if the treatment is instigated quickly. A rehabilitation period of several months must be anticipated if the pain has been in evidence for some months. Emphasis is put on stretching of the anterior thigh muscle. Ice treatment can be repeated every time tenderness is provoked during the rehabilitation period at the apex of the knee cap. Bandage: Some patients have the opinion that the application of tape or bandage around the shin bone directly under the knee cap can relieve the discomfort (tape-description). Complications: In case of lack of progress it should be considered whether the diagnosis is correct or whether complications have arisen. Special consideration should be given to: Special: Since there is a risk that the injury can cause permanent disability, the injury should be reported to your insurance company. |