|
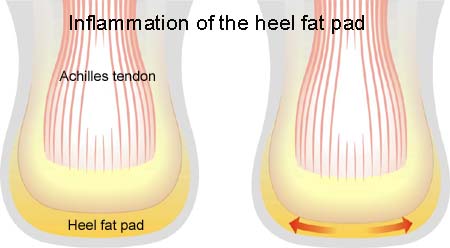
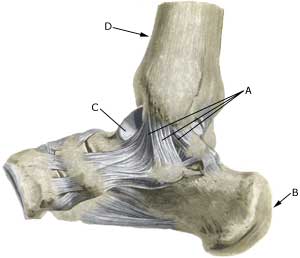
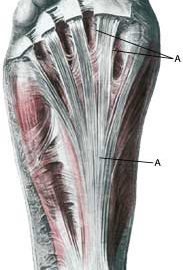
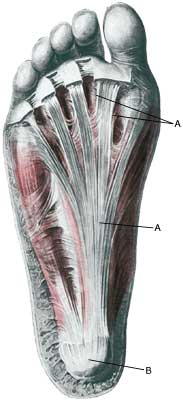
Cause: Occurs after repeated overload in the form of running or jumping. Since the hollow foot tendon is a functional extension of the Achilles tendon, the provoking factors which are instrumental in injuries due to overload of the hollow foot tendon and the Achilles tendon are often the same.
Symptoms: Pain when running and jumping, as well as when applying pressure at the attachment point of the hollow foot tendon directly under the heel bone. The pain is often most pronounced slightly on the inner side of the attachment.
Examination: Medical examination is not necessarily required in slight, early cases where the tenderness is slowly increasing without sudden worsening. A normal medical examination is usually sufficient in order to make the diagnosis, and in all cases when there is a sense of a “crack”, or sudden shooting pains in the tendon, medical attention should be sought as soon as possible to exclude a (partial) rupture of the hollow foot tendon and bone fracture. This situation is best determined by use of ultrasound scanning (or MRI examination). In cases where satisfactory progress is not in evidence, an ultrasound examination should be performed. Ultrasound scanning enables an evaluation of the extent of the change in the tendon; inflammation of the tendon (tendinitis), development of cicatricial tissue (tendinosis), calcification, Inflammation of the tissue surrounding the tendon (peritendinitis), as well as (partial) rupture (article) (Ultrasonic image).
Treatment: Rest from the painful activity (running). The injury can in some cases heal within a few weeks if treatment is commenced at an early stage (article). If the pain has been present for several months, and especially if ultrasound scanning reveals thickening and change in the tendon, a rehabilitation period of several months must be anticipated. It is imperative that the footwear is in order, with good running shoes including shock absorbing heels. Pressure on the hollow foot tendon can be relieved by walking in shoes with an arch support. Treatment with ice can be repeated every time the hollow foot tendon becomes tender during the rehabilitation phase. Injection of corticosteroid is not appropriate in the course of treatment (article).
| Rehabilitation of children and adolescents: INSTRUCTION |
|
|
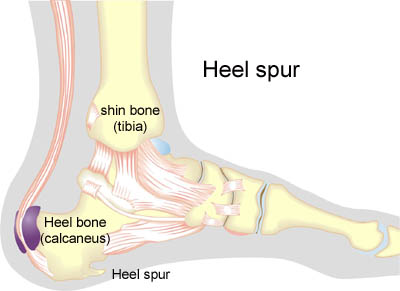
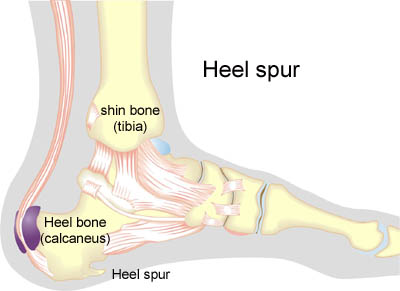
Heel spur: Inflammation of the hollow foot tendon is occasionally connected to a heel spur. A heel spur is a new bone development which is seen in connection with a prolonged Inflammation at the point of attachment of the hollow foot tendon on the heel bone due to overload. A heel spur is thus a consequence of an injury due to overload, and not the cause. If a heel spur has developed, it will never disappear. Heel spurs have no practical significance, and require no treatment. Many symptom free athletes have heel spurs without having had symptoms from the point of attachment of the hollow foot tendon. Surgical removal of heel spurs as performed in earlier days is now virtually no longer used
Bandage: Taping to relieve problems with the hollow foot tendon is of questionable significance, but can be attempted as the tape will not invoke further injury if applied in the correct manner (tape-instruction).
Complications: If there is not a steady improvement in the condition a medical examination should be performed to exclude:
- bone fracture in the foot
- stress fracture
- inflammation of the bursa
- bone membrane tear (periosteal avulsion)
- inflammation of the tendon sheath
Special: As prolonged overload or strain on the hollow foot tendon has a large risk of developing in to chronic Inflammation, which is extremely difficult to treat, it is important to prevent the injury from arising or recurring. The principles in “Rehabilitation, general” should be followed to ensure that quickly increasing training loads at the season start, or after an injury period, are avoided. It is important that running shoes fit well (tight heel cap, shock absorbing soles ). It is vital that the first signs of tenderness or pain are reacted upon, to enable the training to be adapted before the injury reaches the stage where continuing the sports activity may be at risk.
|