|
||
|
||
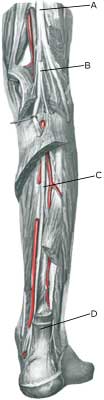
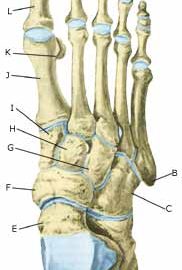
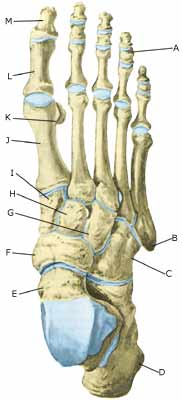
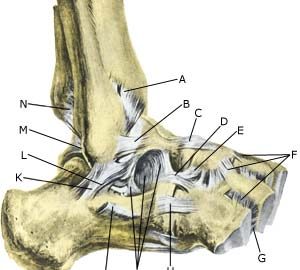
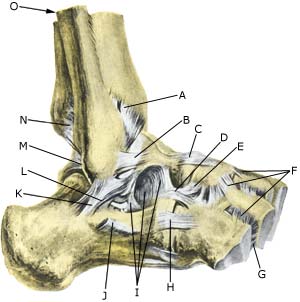
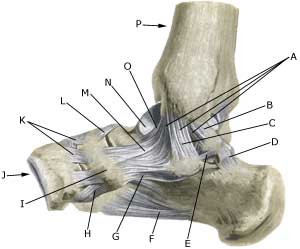
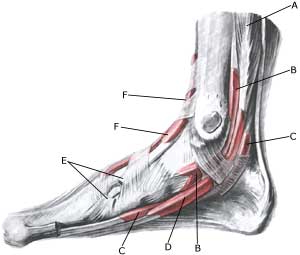
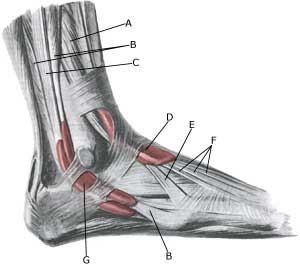
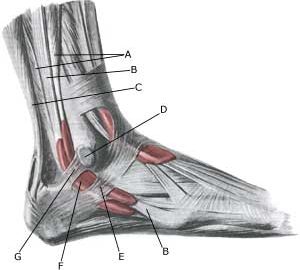
| Cause: The nerve (N tibialis) behind the inner ankle knuckle (mediale malleol) can become jammed against the bone, whereby nerve damage can occur. A great many causes of nerve entrapment have been described (article).
Symptoms: A burning, prickling sensation is felt in the sole of the foot and the toes, often localised to the inward side of the foot. There can be symptoms from the calf. The pain is aggravated when walking and running. The heel is not affected. Examination: Medical examination is usually sufficient to make the diagnosis, as the symptoms can be provoked by applying pressure to the nerve behind the inner ankle knuckle (mediale malleol) (article). The pain will diminish with use of a local anaesthetic above the nerve (diagnostic blockade). If the physician has doubts about the diagnosis, it can be confirmed by use of an EMG examination (ElectroMyoGraphy) Treatment: Treatment primarily comprises relief from the pain inducing activities (running). Use of shoes with a high heel often alleviates the pain. If smooth progress is not achieved by relief and rehabilitation, the treatment can be supplemented by medicinal treatment in the form of rheumatic medicine (NSAID) or injection of corticosteroid in the tarsal tunnel. If the desired effect is not forthcoming, surgery can be attempted to release the nerve, however, the results are often disappointing (article). Complications: If there is not a steady improvement in the condition, medical assistance should be sought to determine whether the diagnosis is correct or whether complications have arisen, with consideration being given to: |