| Diagnosis: |
(Tenosynovitis) |
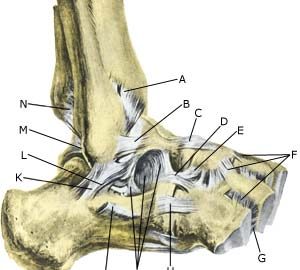
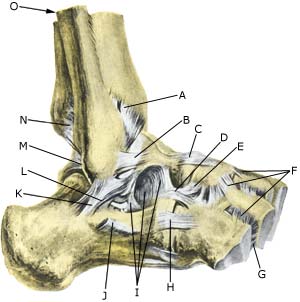
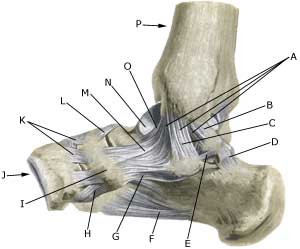
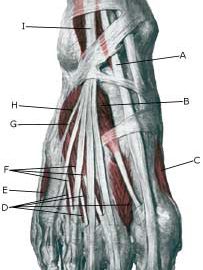
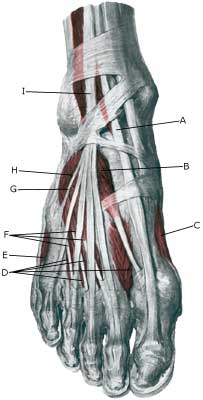
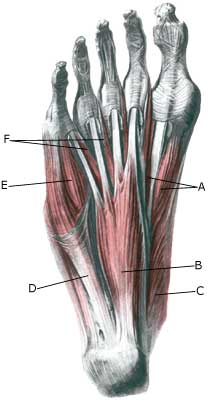
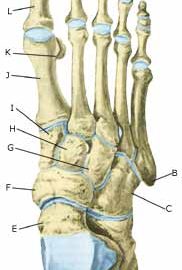
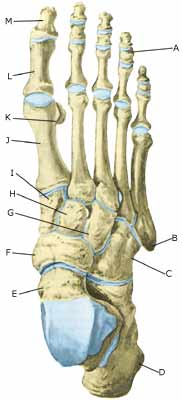
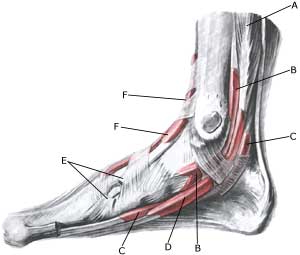
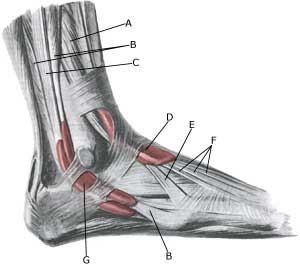
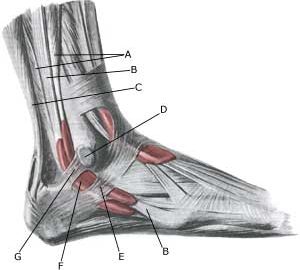
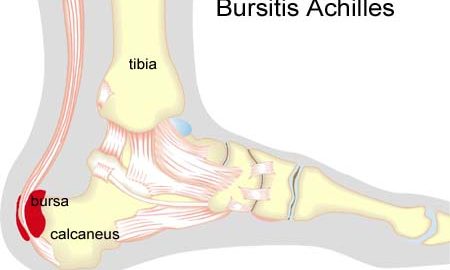
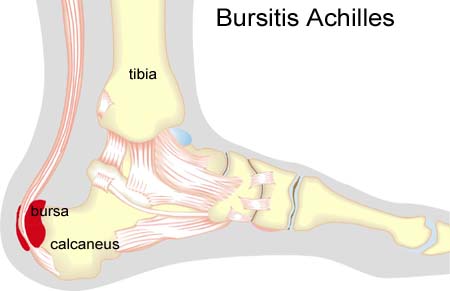
Anatomy: Tendons from the shin bone to the foot pass both inwardly, outwardly, in front and behind the ankle joint, and continue on the back of the foot and the sole to the toes. The tendons are during part of the course deposited in synovial sheaths. |
| Cause: Inflammation of the tendon sheath (tenosynovitis) occurs either due to a mechanical irritation (e.g. a shoe tied too tightly, or from a kick), or often from a straining of the ligaments in the ankle joint. In some cases, a prolonged inflammation of the tendon sheath can cause a weakening, and in worst cases a rupture of the tendon. Inflammation of the tendon sheath is often seen as a result of ligament injuries (article), but is often unfortunately overlooked, (article). The tendon sheaths surrounding the ankle often communicate with the ankle joint itself, and accumulation of fluid in the tendon sheaths can therefore be a consequence of increased fluid in the ankle joint itself, concentration of fluid in the joint (traumatic arthritis / synovitis).
Symptoms: Inflammation of the tendon sheath causes pain along the tendon sheath itself, which is aggravated by stretching and activation of the muscle tendon.
Examination: In obvious cases the diagnosis can be established from a normal medical examination. The diagnosis is, however, easily determinable by use of ultrasound scanning, which can also be advantageously used in cases where steady improvement is not noticeable from relieving the affected area (Ultrasonic image).
Treatment: Treatment is primarily based on relieving the affected area and removal of the provoking factor, if such a factor is in evidence (i.e. tightly bound shoes). If satisfactory progress is not made, the treatment can be supplemented by medicinal treatment in the form of rheumatic medicine (NSAID) Alternatively, draining and evaluating fluid form the tendon sheath can be performed, and injection of corticosteroid into the tendon sheath. Injection into the tendon sheath is best performed if ultrasound guided.
Rehabilitation: Rehabilitation is completely dependent upon which tendon is involved, and whether the inflammation of the tendon sheath is a part of another injury (ligament rupture). The guidelines above (rehabilitation, general) should be followed. Strenuous exercises can be gradually resumed when the pain has decreased.
Complications: If there is not a steady improvement in the condition consideration must be given as to whether the diagnosis is correct, or if complications have arisen:
Special: Shock absorbing shoes or inner inlays will reduce the risk of various forms of inflammation of the tendon sheath. In the event of unsatisfactory progress, or relapse after successful rehabilitation, consideration must be given to performing an analysis of the patient’s running style to establish whether a correction of the running style should be recommended. |