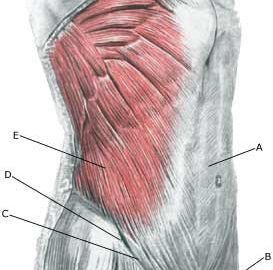
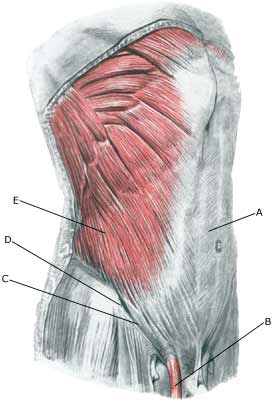
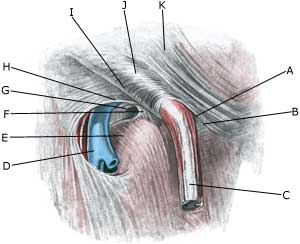
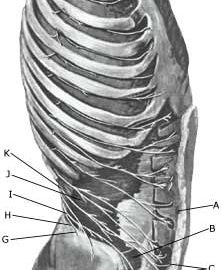
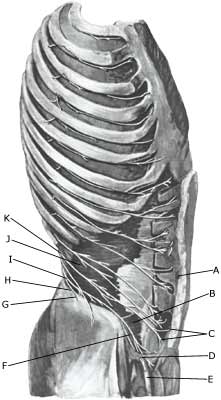
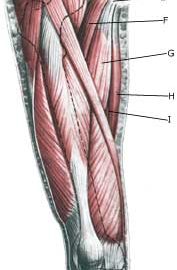
| Cause: Inflammation of the tendon (tendinitis) occurs upon repeated uniform (over)loads. Microscopic ruptures can thus occur in the tendon and in particular at the point of attachment, which causes inflammation. Inflammation of the tendon is a warning that the activity is too strenuous on the particular muscle tendon, and that if the load is not reduced a rupture may occur with a significantly longer subsequent rehabilitation period. The adductor longus muscle, which feels like a firm string in the groin, is one of the adductor muscles, that are most frequently damaged. The muscle is especially susceptible to injury in sports characterized by activity with sprinting with sudden directional changes, a lot of weight training and modest agility training (soccer, hockey), while it is very rarely seen in sports where there is typically great agility (gymnastics). In some cases the inflammation can spread to the fastening of the abdominal muscle on the pubic bone and to the pubic bone joint (symphysis).
Symptoms: Pain when applying pressure along the tendon, worsening upon stretching and activation of the muscle tendon (closing of stretched legs against resistance).
Acute treatment: Click here.
Examination: In light cases medical examination in not necessarily required. Severe cases or cases not improved by treatment should be evaluated by a doctor so that a precise diagnosis can be made. A normal medical examination is usually sufficient in order to make the diagnosis. If in the medical examination there is pain when applying pressure on the muscle attachment point in the groin, and aggravation at the same location upon stretching and activation of the adductor, there is hardly any doubt about the diagnosis. The diagnosis of groin pain can be particularly difficult (article) However, if there is any doubt concerning the diagnosis an ultrasound scan can be performed. Ultrasound is well suited to evaluate the muscles in the area.
Treatment: Since tendinitis of the adductor (M adductor longus) in the thigh is one of the sports injuries with the highest risk of becoming chronic, it is imperative that treatment starts as soon as the first symptoms are felt (and not after months of increasing discomfort). The treatment involves relief, stretching and slowly increasing load within the pain threshold (article). Ice treatment should be used after training if tenderness is felt in the groin. If there is a lack of progress with relief and rehabilitation, medical treatment in the form of rheumatic medicine (NSAID) or the injection of corticosteroid around the inflamed part of the tendon may be considered. The injection of corticosteroid is always part of long-term rehabilitation of a very serious chronic injury. It is therefore necessary that the rehabilitation period after the injection treatment stretches over several months to reduce the risk of relapse and ruptures. The tendon can naturally not sustain maximal load after a long-term injury period and only a short-term rehabilitation period. It is not unusual for rehabilitation to stretch over six months, before maximal load in the form of running with directional change is permitted. In cases where there is lack of progress after rehabilitation and conservative treatment, operative treatment can be attempted. The long-term results of operations are often disappointing.
Complications: If satisfactory progress is not achieved, it should be considered whether the diagnosis is correct or whether complications have arisen. In particular the following should be considered:
Special: Shock absorbing shoes or indlays will reduce the load in the groin. In case of lack of progress or relapse after successful rehabilitation, a running style analysis can be considered to evaluate whether correction of the running style should be recommended. |