|
||
|
||
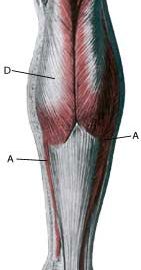
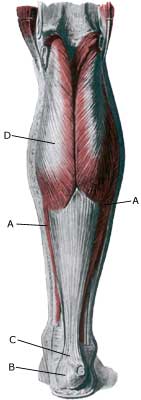
| Cause: With rapidly increasing training of the calf muscles, the muscles can grow so fast that the muscle membranes surrounding the muscles can not keep up with the expansion, thereby increasing the pressure in the muscle group. The pressure can become so high that an impingement of blood vessels and nerves can occur. In some cases chronic compartment syndrome is due to scar tissue formation in the muscle (after earlier muscle ruptures).
Symptoms: With the chronic compartment syndrome, there is slowly insetting pain in the muscle after a few minutes activity. There is a sensation that the muscle is “tightened” and becomes hard, which is accompanied by discomfort. If the activity is stopped the discomfort diminishes, but returns a short period after the resumption of sports activity. Examination: The diagnosis is made on the basis of the characteristic history and possibly with a pressure measurement in the muscle compartment (article). Treatment: With the chronic muscle compartment syndrome the treatment comprises relief and slowly increasing training intensity, rheumatic medicine (NSAID) and massage (article). If there is scar tissue in the muscle, ultrasound guided injection of corticosteroid around the scar tissue formation can be attempted. In cases where there is a lack of progress a surgical splitting of the muscle membranes can be performed, which is usually a minor procedure with good results The rehabilitation is completely dependant on which muscle groups are affected. The sports activity can generally be slowly resumed once pain has diminished, under the principles mentioned under rehabilitation, general. |