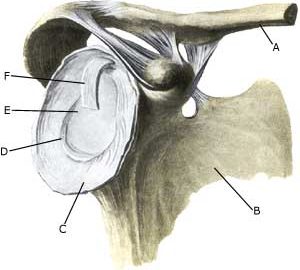
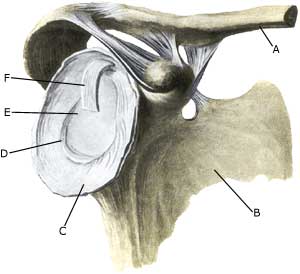
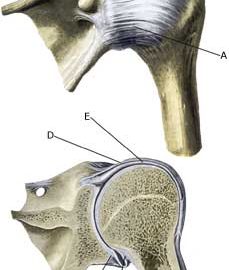
MENISCUS LESION IN THE SHOULDER
|
||
|
||
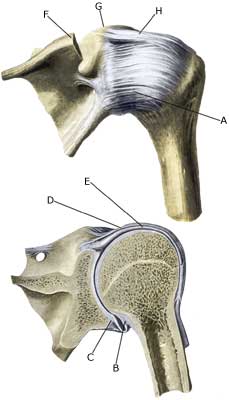
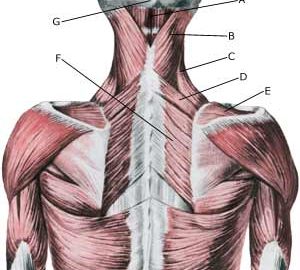
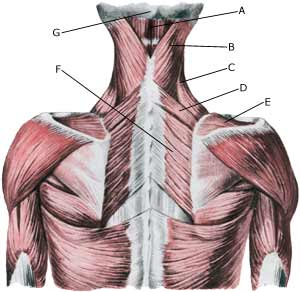
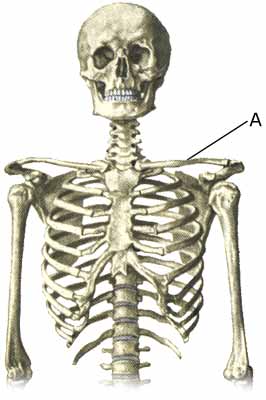
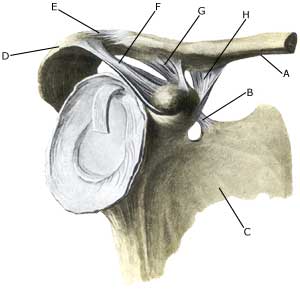
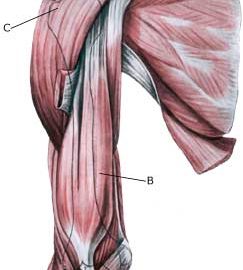
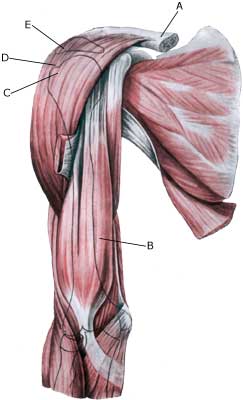
| Cause: In case of repeated (over) loading or in case of one excessive load, the meniscus (labrum glenoidale) may rupture or be ripped from its attachment on the articular surface. After dislodging of the meniscus it may be squeezed in the joint. Lesion of the meniscus is often combined with (partial) ruptures of the shoulder blade muscles: Rupture of the upper shoulder blade muscle, Rupture of the lower shoulder blade muscle and in case of luxation in the shoulder and may occur as the result of a fall, where you break the fall with an outstretched arm or if handball players are “grabbed in the arm” in the moment of shooting (article). There are several different meniscus lesions. Symptoms: Pain in the shoulder joint with certain movements. A sense of something “slipping” in the joint is common. Acute treatment: Click here. Examination: A suspicion of a meniscus lesion in the shoulder (“slipping sensation”) and lack of progress should always lead to a medical examination (Apprehesion test, relocation test). An impression of the meniscus can be formed with MR and ultrasound scan, but the lesion is best assessed using arthroscopy (telescopic examination of the shoulder joint), where treatment can be performed at the same time. Treatment: A referral to arthroscopy is advised where there is a suspicion of a meniscus lesion and smooth progress is not achieved with relief and rehabilitation, where it will be possible to determine the diagnosis, and whether it is possible to stitch the meniscus in place or whether parts of it should be removed. The results of the operation in cases of isolated meniscus lesion are usually good (article). Complications: If progress is not smooth, it should be considered whether the diagnosis is correct or whether complications have arisen. Amongst others the following should be considered:
|