| Diagnosis: |
(Ruptura traumatica ligamenti medialis pedis) |
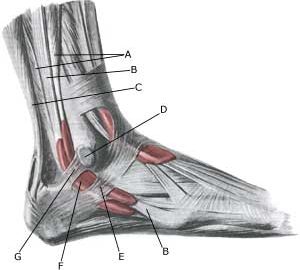
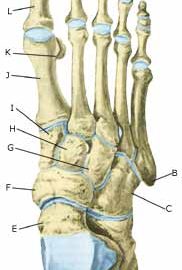
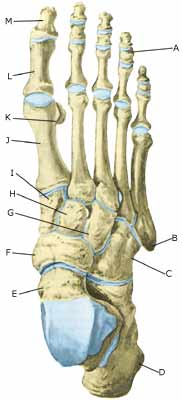
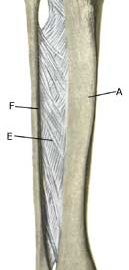
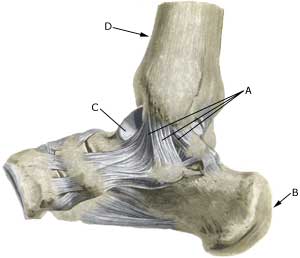
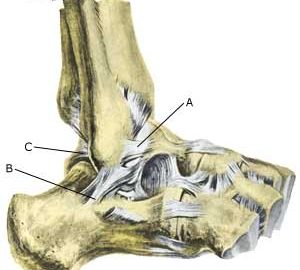
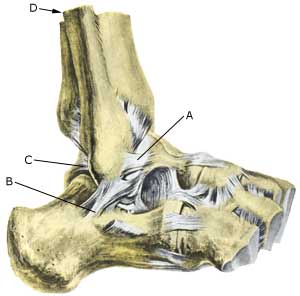
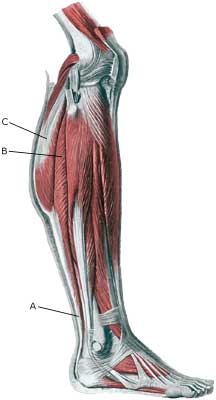
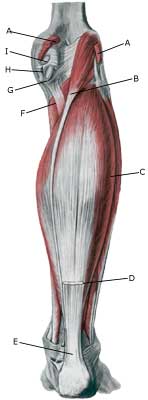
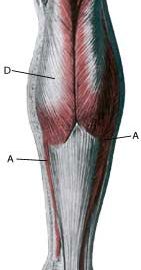
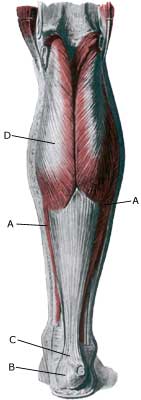
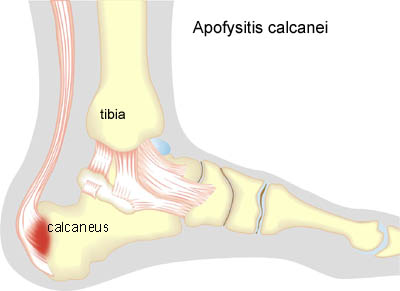
Anatomy: The ankle joint is stabilised by a wide fan shaped ligament on the inside (ligamentum deltoideum), and a set of outer ligaments (fore, centre, and at the rear). The ligaments stabilise the ankle joint, especially when twisting and running with sudden directional changes (Photo). |
| Cause: A rupture of the of the inner ligaments in the ankle joint arises if the foot is twisted such that the ligaments are overstretched and finally rupture. In slight cases the injury can be termed a strain or sprain, and in more serious instances as full or partial rupture or tear. Consequential injuries are often associated with ligament ruptures, amongst others concentration of fluid in the joint (traumatic arthritis/synovitis)and inflammation of the ankle joint tendon sheath, (article), however, these are often unfortunately overlooked (article).
Symptoms: Pain on and under the inner ankle bone (malleolus medialis), swelling due to bleeding, pain when walking.
Acute treatment: Click here.
Examination: Medical examination is not necessarily required for very minor cases (slight sprain) with only minimal swelling and no discomfort when walking. The extent of the swelling is, however, not always a mark of the degree of the injury. Medical examination is recommended with more extensive swelling or pain, in order to eliminate bone fracture in the ankle and a rupture of the ligament between the shin and calf bones (syndesmosis rupture). A normal medical examination is usually sufficient in order to make the diagnosis. X-ray examination should be performed in all cases where there is a suspicion of a bone fracture or syndesmosis rupture. Vigorous twisting of the ankle in the acute stage to appraise the degree of looseness is not indicative, as this has no influence on the choice of treatment (article). Ultrasound examination will give valuable information when the ligament is ruptured (Ultrasonic image).
Treatment: Treatment of ligament injuries is today conservative (rehabilitation). Many patients have earlier undergone operations and setting of plaster cast, however, this course of treatment has practically been abandoned in relation to uncomplicated ligament ruptures (article).
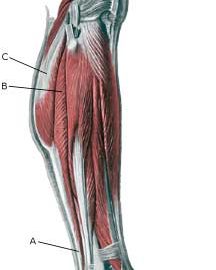
Bandage: It is recommended to use tape in the course of rehabilitation when starting to run on an uneven surface, or with sudden directional change. Nerve cells (proprioreceptors) in the ligaments transmit information to the brain on the position of the ankle joint. The brain sends information to the muscles, which are activated, ensuring that the ankle is held correctly. The nerve paths do not function in an optimal manner when the ligament is injured, and the risk of a new twist of the foot is increased thereby. Use of tape is primarily designed to stimulate the small nerve cells in the skin, thus enabling these to act as a substitute for the nerve cells temporarily damaged in the ligament. The function of the tape is thus not a pure mechanical stabilising of the ankle joint (tape-instruction). In some cases, certain forms of bandaging around the ankle can be used to advantage.
Complications: If there is not a steady improvement in the condition consideration must be given as to whether the diagnosis is correct, or if complications have arisen:
It is extremely rare that the injury results in a chronically loose ankle joint if rehabilitation is handled sensibly. If the injury does result in a chronically loose ankle joint, intensive co-ordination training must be recommended. Bandages can be tried if this is not sufficient, and if this still does not give the desired effects, surgical intervention to tighten the ligaments can be attempted.
Special: Seesaw exercise is important in the rehabilitation phase, as well as in a preventive capacity. As a preventive measure, seesaw exercises should be performed frequently throughout the rest of the active sporting career if ligament injuries in the ankle joint have previously been experienced. Begin by standing with both feet on the seesaw and use hands for support on the wall. Gradually let go of the support to finally train by standing on only one leg (article). Special bandages have in some studies been shown to reduce the risk of ligament injuries.
(article-1), (article-2). |