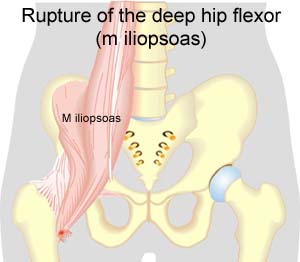
RUPTURE OF THE DEEP HIP FLEXOR
|
||
|
||
 |
||
| Cause: When a muscle is subjected to a load beyond the strength of the muscle (jumping, kicking), a rupture occurs. The vast majority of ruptures are partial muscle ruptures.
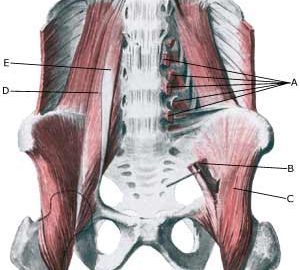
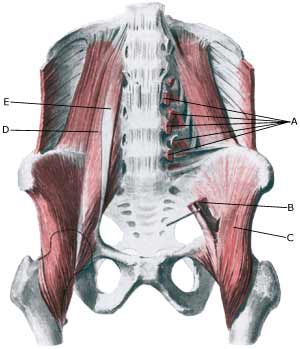
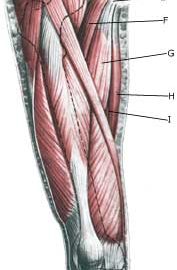
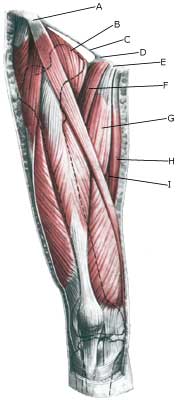
Symptoms: In light cases a local tenderness is felt after the load (“sprained muscle”, “imminent pulled muscle”) e.g. kicking a ball with the instep. In severe cases a sudden shooting pain is felt in the muscle (“partial muscle rupture”, “pulled muscle”) and in the worst case a violent snap is felt, rendering the muscle unusable for e.g. walking up stairs (“total muscle rupture”). With muscle injuries the following three symptoms are characteristic: pain upon pressure, stretching and activation against resistance. In some cases the bleeding can be so great that it entraps the nerve to the bone (nervus femoralis) with increasing pains, reduction of power and symptoms into the leg (article). Acute treatment: Click here. Examination: In light cases with only minimal tenderness and no discomfort when walking normally (“sprained muscle”, “imminent pulled muscle”), medical examination is not necessarily required. The severity of the tenderness is, however, not always a measure of the extent of the injury. In case of more pronounced tenderness or pain medical examination is required to ensure the correct diagnosis and treatment. A normal medical examination is usually sufficient in order to make the diagnosis, however, if there is any doubt concerning the diagnosis an ultrasound scan can be performed. It is known that the larger the bleeding is assessed in the ultrasound scan, the longer the rehabilitation period (Ultrasonic image), (article). Treatment: The treatment usually consists of relief and careful rehabilitation (article). Only in very rare cases is surgery indicated (e.g. in case of total ruptures or very heavy bleeding). Complications: In case of lack of progress it should be considered if the diagnosis is correct or whether complications have arisen. In particular the following should be considered:
|