|
||
|
||
| Cause: Rupture of the anterior cruciate ligament usually occurs during running with fast changes of direction or as the result of a fall while skiing. Most injuries occur without contact with an opponent. Cruciate ligament injuries in adolescents are being diagnosed with increasingly regularity.
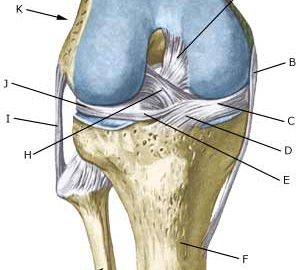
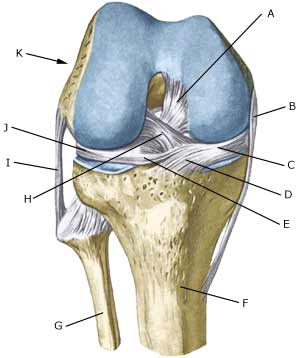
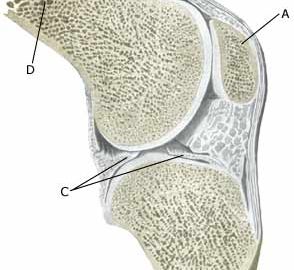
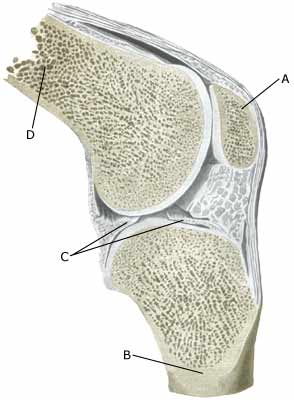
Symptoms: Usually a snap can be heard or felt and continued sports activity must be aborted. The knee swells within the first few hours, after which the knee can not bend completely. You can subsequently often sense that the leg gives way (knee failure). Acute treatment: Click here. Examination: If a partial or complete rupture of the cruciate ligament is suspected, you should seek medical attention (casualty ward) immediately, to obtain a diagnosis. The doctor can perform various tests on the knee (front drawer looseness, Lachmann Pivot shift) to examine the stability of the knee. It should be noted that the looseness in the knee can often only be demonstrated after two weeks. The fluid in the knee can be drained. Blood in the knee provides a very strong suspicion of a rupture of the anterior cruciate ligament. The examination is often more difficult in adolescents. The bleeding that occurs after a rupture of the anterior cruciate ligament can usually be seen in an ultrasound scan (Ultrasonic image) (article) or MR-scan. Arthroscopy (a telescopic examination of the knee) is the best suited examination if there is any doubt in the diagnosis. Treatment: Caution will normally be exercised regarding operating on children in the pre-teenage age group, however, teenagers nearing a fully grown state will usually be advised surgery with the insertion of a new cruciate ligament (article-1) (article-2) (article-3). An intensive rehabilitation period of at least six months is to be expected. It is important that the knee is stretched completely at least twice a day. The surgeon should be consulted if problems occur with stretching the knee completely Bandage: Hinge bandages (Don-Joy) can be utilised the first few weeks. Tape treatment of cruciate ligament ruptures in the knee has no sure effect. Complications: In case of lack of progress you should consider various complications:
In cases where the knee cap tendon is used as a new cruciate ligament an inflammation is often seen where the knee cap tendon has been removed (article).
|