|
||
|
||
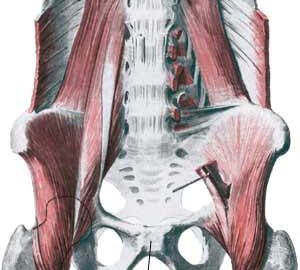
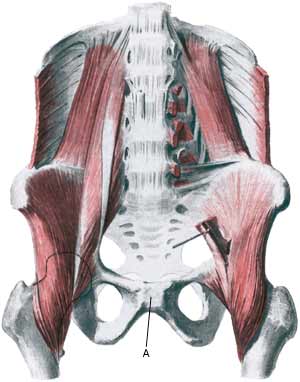
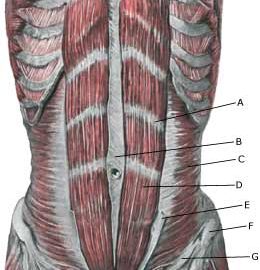
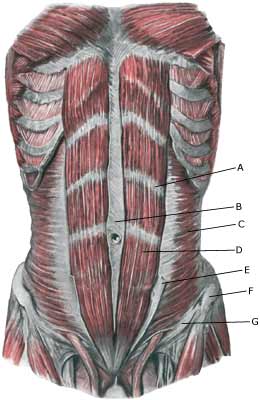
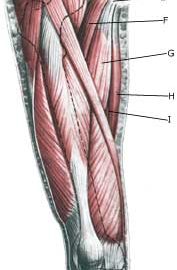
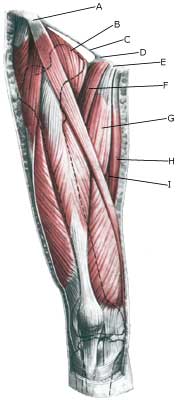
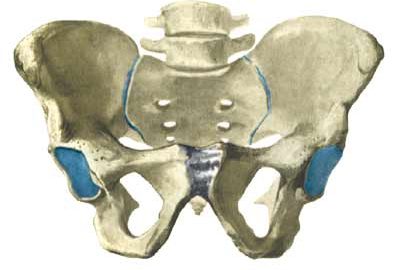
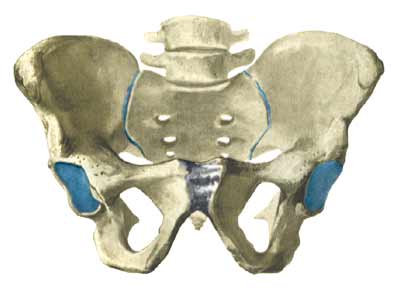
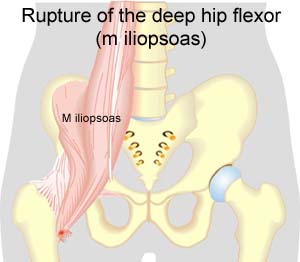
| Cause: occurs in the joint, whereby the joint can become loose so that the two halves of the pelvis can move slightly in relation to one another due to heavy loads. (In many areas the symptoms are the same as those seen in pregnant women with pelvic loosening). The inflammation is a warning that the training is too strenuous, and that if the load is not reduced a chronic condition with a significantly longer rehabilitation period may follow. Inflammation of the pubic joint is often preceded by long-term inflammation of the abdominal muscle fastening on the pubic bone and inflammation of the adductor muscle of the thigh. Inflammation of the pubic joint (osteitis pubis) is especially seen in sports characterised by activity with sprinting with sudden changes of direction (soccer, ice hockey).
Symptoms: Pain around the pubic bone, the abdominal muscle fastening and in the groin. Aggravated with asymmetric loads (jumping on one leg). Acute treatment: Click here. Examination: Inflammation of the pubic bone joint is always an athletically serious condition that always requires medical examination. A normal medical examination is usually sufficient in order to make the diagnosis. Tenderness will often be present on the pubic bone joint (direct and indirect). The examination can be supplemented with X-ray, scintigraphy, MRI- and ultrasound scan. The diagnosis of groin pain can be particularly difficult (article) Treatment: Inflammation of the pubic bone joint is often the end stage of a poorly treated chronic overloading of the muscle fastenings on the pubic bone and the groin. In severe cases the rehabilitation period can be expected to last a year (and in the worst case render a return to sports an impossibility). It is therefore of the utmost importance that the treatment be started as soon as possible, without continuing the condition inducing sports activity. The treatment primarily consists of relief and subsequently slowly increasing training of the musculature around the pubic bone joint (stomach, groin), pelvis and loin. In case of lack of progress with rehabilitation, a medical treatment can be considered in the form of rheumatic medicine (NSAID) or the injection of corticosteroid around the inflamed tendon fastening or in the pubic bone joint (article). The injection can advantageously be ultrasound guided. Since the injection of corticosteroid always is part of a long-term rehabilitation of a very serious, chronic injury, it is decisively necessary, that the rehabilitation course stretches over several months to reduce the risk of relapse. A rehabilitation period of ½ – 1 year before maximum load in the form of maximal running with directional change is allowed is not unusual. Some have tried operating for this condition, which usually returns to normal when the load (sports activity) ceases (article). Particularly careful consideration should be made before accepting a surgical offer with the risks this entails, for a condition that does not threaten mobility nor health (article). Complications: If progress is not smooth the correctness of the diagnosis should be considered. In particular, the following should be considered:
Special: Shock absorbing shoes or inlays will reduce the load in the groin. In case of lack of progress or relapse after successful rehabilitation, a running style analysis can be considered to evaluate whether correction of the running style should be recommended. |